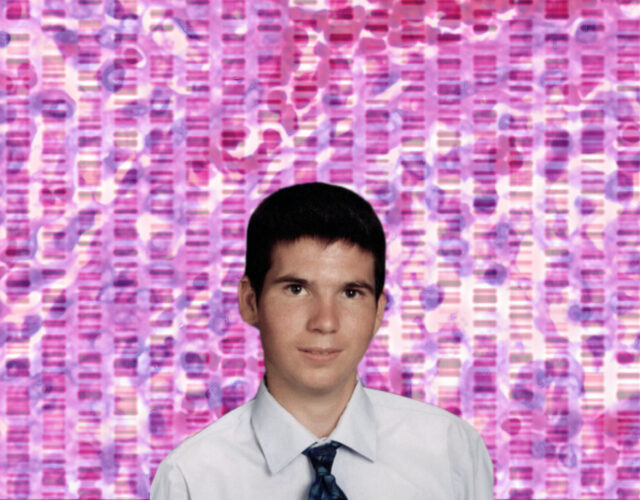
By all accounts Jesse Gelsinger was a sweet, sharp-witted, if not particularly ambitious kid who loved motorcycles and professional wrestling. In 1999 he was living in Tucson, Arizona, with his parents and siblings, attending high school, and working part-time as a supermarket clerk. As he got older, he became more independent and, like many teens, a touch rebellious; in his case that led to life-threatening health problems.
Jesse had a rare metabolic disorder called ornithine transcarbamylase deficiency syndrome, or OTCD, in which ammonia builds up to lethal levels in the blood. Babies born with OTCD usually fall into comas soon after birth and suffer brain damage. Half of them die within a month. Jesse’s milder version of the deficiency was diagnosed when he was two years old, and he managed the condition with a low-protein diet and a regimen of nearly 50 pills a day.
Still, he had occasional health crises. When he was 17, he stopped taking the drugs regularly. One day his father came home to find him curled up on the couch, vomiting uncontrollably. He had to be intubated and kept in an induced coma until his ammonia levels were brought under control.
So when a doctor told Jesse that a clinical trial for a potential OTCD treatment was in the works, he was very interested. Researchers at the University of Pennsylvania in Philadelphia were developing a fix for the OTC gene, which produces an enzyme that prevents ammonia buildup. Patients would be injected with working copies of the gene that had been attached to an adenovirus, a type of cold virus. The virus, altered to be harmless, would infect the patients’ liver cells and integrate the added gene into their chromosomal DNA.
The field of gene therapy had so far helped just a few people with genetic diseases. But the researchers’ experimental treatment had lengthened the lives of lab mice bred to be deficient in OTC enzymes, and the scientists were hopeful the gene-repair method they were testing could eventually be used to treat many liver diseases. The trial Jesse would join was a safety study, aimed at moving toward a treatment for babies with OTCD, and was not intended to improve the participants’ health. But Jesse was eager to help, and he flew to Philadelphia in September 1999 to take part.
Jesse was the 18th person to receive the modified virus. Previous patients in the trial had experienced flu-like symptoms, but he had a much worse reaction. Within a day he became disoriented and showed signs of jaundice. He had an intense inflammatory response and developed a dangerous blood-clotting disorder, followed by kidney, liver, and lung failure. Four days after receiving the shot Jesse was declared brain dead and taken off life support. The team of doctors and nurses caring for him were stunned by his rapid decline and death.
The news that an experimental treatment had killed a basically healthy volunteer rocked the field of gene therapy and the broader world of biological research. News coverage portrayed the trial researchers as overeager and undercautious, taking shortcuts and disregarding rules meant to protect the people in their care.
“The death is the latest in a series of setbacks for a promising approach that has so far failed to deliver its first cure and that has been criticized as moving too quickly from the laboratory bench to the bedside,” the Washington Post reported, in the first of many articles about Jesse’s death and the ensuing crisis it set off.
In a flash the field of gene therapy collapsed, taking its grandiose promises of miracle cures along with it.
Biochemist Jennifer Doudna, who later discovered the CRISPR-Cas9 gene-editing mechanism, remembers feeling the shock waves as a young researcher, even though her work had nothing to do with gene therapy or any kind of medical research.
“We were all very much aware of what happened there and what a tragedy that was,” she said in a recent interview. “That made the whole field of gene therapy go away, mostly, for at least a decade. Even the term gene therapy became kind of a black label. You didn’t want that in your grants. You didn’t want to say, ‘I’m a gene therapist’ or ‘I’m working on gene therapy.’ It sounded terrible.”
Of course, the field eventually rebounded. In the 20 years since Jesse’s death, private and public ventures have invested billions of dollars in efforts to cure diseases by altering or replacing our faulty genes. To date, these efforts have produced just a few marketable medicines—two therapies for lymphoma, a treatment that reverses a form of inherited blindness, and most recently, a therapy for spinal muscle atrophy. But innovation has accelerated in the past few years thanks to CRISPR, which has enabled highly targeted editing of genes that is vastly cheaper and quicker than earlier methods. Treatments for hemophilia, muscular dystrophy, and other genetic diseases now seem almost within reach.
Scientists say this new generation of gene-therapy research is safer. But how safe is safe enough? How much risk is acceptable, how can researchers assess the risks, and who should bear them?
Investigating the Investigators
In the weeks after Jesse’s death James Wilson, the director of the University of Pennsylvania’s Institute for Human Gene Therapy, and the other doctors involved in the trial tried to understand what happened. They focused on the possibility that the adenovirus had triggered a fatal immune response for reasons that were not yet clear.
Meanwhile, journalists and federal health officials discovered several troubling lapses in the conduct of the study. For example, the researchers had earlier told the FDA they would tighten up the trial’s eligibility criteria, but they never followed through. When two patients suffered serious side effects, the scientists did not immediately inform the agency or put the study on hold as required. It turned out Jesse’s pretrial test results showed he had poor liver function, indicating he arguably shouldn’t have received the OTC gene injection.
But perhaps most damning were failures in the informed-consent process. Researchers hadn’t told Jesse about the earlier patients’ side effects or about two lab monkeys killed by high doses of adenoviruses. If he had been properly briefed about these previous issues, he might have dropped out of the study and still be alive today. Wilson was also accused of a conflict of interest: he had a stake in the company that owned the gene-transfer technology and stood to benefit if the trial succeeded.
Wilson denied that financial considerations affected the study and said it was impossible to predict that Jesse would suffer such a bad reaction. Nevertheless, the Gelsinger family sued, and the university quickly settled for an undisclosed sum, while declining to take responsibility for Jesse’s death. In January 2000 the FDA suspended human research at Penn’s Institute for Human Gene Therapy, and the university eventually shut the program down.

The FDA charged Wilson with several violations, and in 2005 he agreed to restrictions on his human research for five years. The university also paid the federal government a $514,000 settlement.
The investigations drew attention to wider problems in oversight of gene-therapy experiments and human research generally. For example, the FDA and NIH revealed that 691 volunteers in gene-therapy experiments had either died or fallen ill in the seven years before Jesse’s death; only 39 of these incidents had been reported promptly as required. The agencies tightened monitoring of trials, increased inspections, and created a new system for reporting serious side effects, among other steps. Penn responded to the crisis by strengthening the institutional review boards that oversee its trials, putting in new protections for patients, and prohibiting researchers from having financial stakes in their trials.
Yet as the pharmaceutical industry continued growing and its profits soared, demand for test subjects increased, and more research was undertaken by private companies rather than academic or government institutions. That raised new fears that patient safety could be compromised in the rush to get products to market.
“Contrary to hopes of human research reform spurred by Jesse Gelsinger’s death, oversight has flattened, profit motives have become more entrenched in medical research, and the pool of potential human subjects has come to focus on the vulnerable, both at home and abroad,” wrote Osagie Obasogie, a professor of bioethics at the University of California, Berkeley, in 2009. “And the confidence behind recent attempts at gene therapy often exceeds the evidence for its safety and efficacy in humans.”
Putting Safety First
After the government’s investigation, Wilson remained at Penn but fell into a kind of professional disgrace, his career as a leading researcher in tatters. It was a striking reversal for a renowned scientific pioneer. In 1992, in one of gene therapy’s first triumphs, he had successfully treated a woman for extremely high cholesterol, demonstrating that the field could actually improve patients’ lives. Yet a few years later he found himself branded as careless and even dangerous to the people he was trying to save. Wilson briefly considered leaving science entirely. Instead, he turned his focus to understanding why Jesse’s immune system had gone haywire and how to avoid such outcomes in the future.
He and his team concluded that the teenager had probably experienced a rare phenomenon called antibody-dependent enhancement. Jesse had been previously exposed to the adenovirus that was used in the trial, they surmised, which created antibodies that supercharged the subsequent reinfection rather than fighting it. It seemed that altering adenoviruses would perhaps never make them safe enough to put into people.
Wilson turned instead to the study of another class of gene-delivery vehicles called adeno-associated viruses, or AAVs, which were known to provoke little or no immune response.
“I really thought a lot about, should we try to make the more efficient vectors safer, or should we make the safer vectors more efficient?” he said in a phone interview. “We decided to go with the latter—really start from a platform of safety and just incrementally try to make them better. We’ve made a lot of advances in making them better. What you don’t see are all the failed experiments. There are some circumstances where in our attempt to make them more efficient, their safety profile was compromised. So we don’t even bring those forward.”
His research group tested hundreds of AAVs, finding that some penetrate cardiac tissue most efficiently, while others work best for the liver or brain. Those discoveries have been crucial to the production of a new generation of medicines. For example, Editas Medicine, a gene-therapy company based in Cambridge, Massachusetts, uses one of Wilson’s vectors to deliver its treatment for Leber’s congenital amaurosis type 10, an inherited blindness condition. Using that particular virus helps ensure the therapy only penetrates (is trophic for) the vision cells that need to be altered and doesn’t end up causing effects elsewhere.
“We cannot say there’s zero exposure to the rest of the body,” Editas CEO Katrine Bosley said during a talk at the Science History Institute last fall. However, “the virus that we’re using, AAV5, is particularly trophic for photoreceptors.”

AAVs have been used safely in many studies, and last month the FDA approved an AAV-based gene therapy for a lethal disorder for the first time. The drug, Zolgensma, treats spinal muscular atrophy, an inherited disease that destroys nerve cells and is the most common genetic cause of death of infants. In a press release announcing the FDA approval, Wilson said, “This approval is a huge milestone for the rare disease community because the approach can be leveraged across many different diseases.”
But he now balances such celebration with hard-earned prudence. In 2018 Wilson published a paper warning that animals receiving high doses of AAVs in tests of a therapy for spinal muscular atrophy sustained nerve and liver damage, raising questions about the volume of viruses humans can safely handle. Researchers from his lab also reported that AAVs may unexpectedly mutate during the virus-manufacturing process, causing changes in the way they function. The report described a way to stabilize the viruses’ structure.
He has also warned of the pressures that can lead to dangerous errors and oversights. In 2009 he published a cautionary article in response to the first clinical trial that used embryonic stem cells, a technology that, like CRISPR, stoked massive hype over its promise as well as fears of unethical genetic tinkering.
In the essay Wilson urged scientists not to reenact gene therapy’s “hyperaccelerated transition to the clinic” of the 1990s. That ill-fated rush to experiment on human subjects was driven by simplistic modeling suggesting the approach “ought to” work, as well as the “fervent hopes” of charitable foundations seeking cures for lethal diseases, he wrote. He also blamed overenthusiastic scientists, uncritical media coverage, and investors who eagerly funded therapies that weren’t backed by actual results.
“Some would call it kind of irrational exuberance,” he said in his interview with Distillations. “The hope exceeds the science, and expectations are not met.”
Doudna expressed similar concerns about CRISPR.
“I hope that we don’t get ahead of ourselves with this technology. As exciting as it is, I really would like to see . . . people take a very measured and responsible path forward, where there’s careful vetting along the way,” she said. “Of course, the challenge is that patients are waiting, so you don’t want to delay unduly. But you also want to be safe.”
Facing Unknown Risks
Gene therapy had its first success early on, nearly a decade before the OTCD trial. In 1990 doctors partially reversed a case of severe combined immune deficiency, or SCID, also known as “bubble boy syndrome,” in a young American girl, Ashanthi DeSilva. They drew her white blood cells, used a retrovirus to insert a working gene into the cells, then injected them back into her body, which helped give her a functioning immune system.
French researchers conducted a similar trial with 10 children in 2002, using stem cells taken from the patients’ bone marrow. The treatments worked, but within a few years four of the children developed leukemia and one of them died. The retroviral vectors had been integrated near oncogenes, which can cause cancer, apparently triggering the leukemia.

Ashanthi DeSilva, age 6, March 1993. two years after. On September 14, 1990, at the age of 4, DeSilva became the first gene-therapy patient when she was implanted with corrected genes to address her form of severe combined immunodeficiency, often called bubble boy disease.
Reducing the risks of cancer and other harmful effects is a central task of gene-therapy research, but much work remains. Even CRISPR, celebrated for enabling highly specific, targeted genetic edits, still has the potential to go awry.
CRISPR is a fundamentally new way to change genes. The basic technology consists of an enzyme that cuts DNA and a segment of guide RNA that tells the enzyme where to snip. The package may include other components, such as a new piece of DNA code to plug into the edited area. The cell’s natural repair mechanism completes the edit. Scientists can deliver CRISPR using AAVs, as Editas is doing, but that’s not the only option; CRISPR can be encapsulated in bubbles of fat, injected directly into cells, or sent through a hole created by an electric current, among other techniques. Editing is meant to occur when the enzyme comes in contact with the target DNA, and only then.
“The hope that we have now for CRISPR technology is that it literally is a way to program enzymes to go to exactly the place in the DNA where a change is desired, and nowhere else, and make a precise alteration,” Doudna said. “It’s a very different way of altering genomes that is controllable. The potential is clearly very, very exciting.”
But cell biology is complex, and learning how to avoid unintended consequences remains a work in progress. Last year, for example, two groups of researchers said they found a possible problem when they tested CRISPR on retinal cells and stem cells. The intended edits often didn’t work because they triggered a cell’s p53 gene, which responds to DNA damage by telling a cell to self-destruct. The gene plays an important role in keeping mutations from becoming cancerous, yet CRISPR worked better in cells with a dysfunctional p53 gene. In other words, CRISPR apparently subverted one of the body’s disease-fighting mechanisms, making healthy cells die and allowing potentially cancerous ones to remain.
No one has seen lab mice get cancer after CRISPR treatment, but it’s unclear if they have been observed long enough to allow tumors to develop. In the French SCID study, the children were diagnosed with leukemia years after their treatment. Potential long-term side effects are a concern with gene therapies because the treatments are basically permanent; they can’t be washed out of the body the way a conventional drug often can. The discovery of the p53 issue and the uncertainty about its importance are reminders that scientists simply don’t know everything that could happen when CRISPR is put into a human body.
Wilson said the question of whether a gene edit could inadvertently cause mutations elsewhere in the chromosome and cause cancer in a patient, much as SCID gene therapy caused leukemia, will not be resolved soon. “It’s definitely a theoretical concern, and it’s going to be a challenge to quantify what the risk is. That’s going to be a huge challenge,” he said.
That doesn’t mean clinical trials of CRISPR-based therapies shouldn’t happen, but it does affect the risk-benefit calculation, he said. Many patients with devastating diseases, such as muscular dystrophy, cystic fibrosis, and Huntington’s disease, as well as certain cancers and rare diseases for which few treatments are available, will accept the unknown chance they’ll experience some harm from an experimental therapy if it also might lessen their symptoms or extend their lives.
Trials that include such patients are ethically acceptable, whereas the possibility of serious side effects may make trials of less urgent therapies unacceptable. A clinical trial of a CRISPR-based treatment for color blindness, for example, might not be worth the risk.
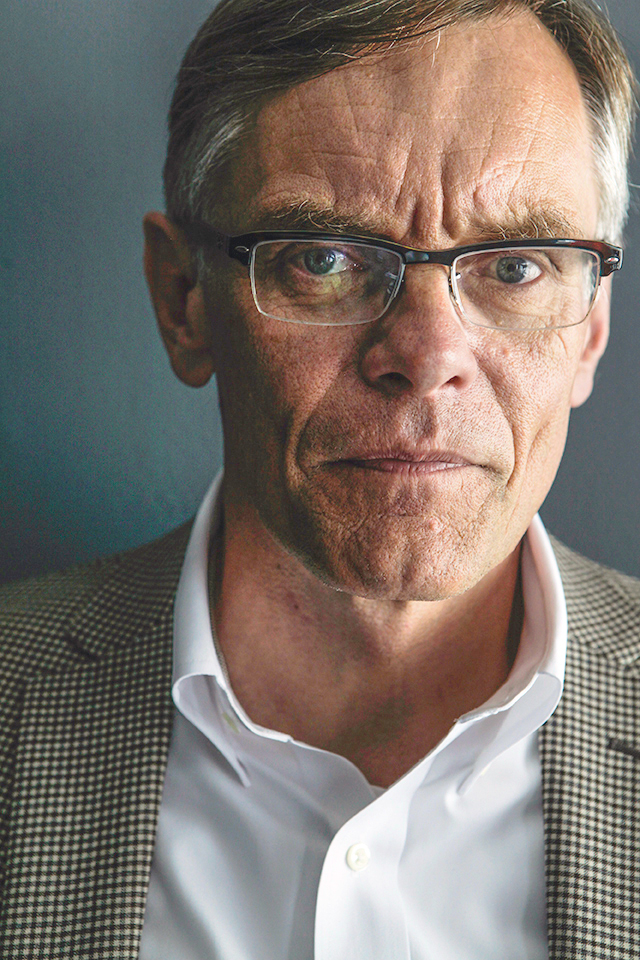
James Wilson, June 2015.
“For [gene] editing you’re going to be focused for a while on diseases in which there is significant unmet need, not a lot of alternatives, and where the risk tolerance would be higher,” Wilson said.
“It’s going to be a long road before we get to the point where editing would be deemed safe enough for diseases other than those that have really significant morbidity and mortality,” he added.
Biotech firms go to great lengths and spend hundreds of millions of dollars trying to make sure their products are effective and safe, but preclinical testing in animals and cell cultures goes only so far. Bosley said during her talk at the Science History Institute that the only way to see if a treatment really works is to put it into a person.
“The genetic context of a mouse or a rat has nothing to do with human genetic context. You just can’t know. You are taking a greater leap into the unknown with these kinds of experimental medicines,” she said.
“The FDA has learned lessons, the industry has learned lessons, and I think we are all seeking to be very careful in how we advance,” she said. Yet “the risk never goes away. That’s what it takes to make new medicines.”