Through her kitchen window Borgny Egeland surveyed grey skies made luminous by a midday sun hanging low on the horizon. The distant sound of the town hall’s chimes might have lightened her spirits, but Borgny had reached her wit’s end.
Her first child, Liv, had been born a healthy, bright-eyed girl. A joy to Borgny and her husband, Harry, Liv was the child they dreamed of when the young couple started their family in late-1920s Oslo. But after three years little Liv had not learned even one word. The family physician reassured Borgny: ”Just give it time,” he said. So Borgny and Harry waited. In the meanwhile they welcomed their second child, a healthy son named Dag. But Dag began showing signs of developmental delay even more quickly than his sister. By 1934 six-year-old Liv could say only a few words and walked with spastic irregularity. At four, Dag could not speak and was unable to walk, eat, or drink on his own.
Borgny visited a number of medical specialists, herbalists, and even a psychic healer. Why, she asked, had her healthy babies gradually, inexorably fallen into profound mental disability? No one had an answer. Curiously, the children gave off a strong musty odor from their hair, skin, perspiration, and urine. Their asthmatic father could barely tolerate it.
As well as struggling with her children’s disabilities, Borgny was struggling against doctors’ dismissive views of “feeblemindedness.” Mentally disabled people were considered hopeless cases, suffering from a defect of the brain caused by bad genes and destined to be warehoused in mental institutions alongside patients with psychiatric disorders, epileptics, and others whose “bad brains” were beyond the help of modern medicine.
This attitude was about to change. A chance conversation connected Borgny’s husband to Asbjørn Følling, a doctor who had worked on high-altitude metabolism and physiology in the mountains of Colorado. His unusual dual background in chemistry and metabolic medicine would prove crucial: the disease he was about to discover would open up a new view of cognitive disability and inherited disease.
In 1934, as the frigid Oslo winter finally yielded to the coming of spring, Følling, professor of nutritional research at Oslo University Hospital, agreed to an appointment with Borgny, but with no expectation of being able to help her. “I examined the children mainly because I did not want to be hostile to the mother,” he later recalled. He performed a full physical examination and found nothing remarkable, except for their unmistakable “feeblemindedness.” Følling then examined the children’s urine, working from his own improvised laboratory in the attic of the medical ward. He checked the urine samples first visually and then chemically for acidity, pus, protein, and glucose. Protein or glucose in the urine would have suggested kidney malfunction, especially diabetes. But all the tests were negative. Except for the musty odor, the urine seemed perfectly normal.
Følling faced the same impasse that had confronted all the previous physicians, including his own colleagues at the Oslo hospital, who had thoroughly examined Dag on previous occasions. But unlike the others Følling tried another test: he added a few drops of acidified ferric chloride solution to each urine sample. This test, sometimes called Gerhardt’s test, was commonly used to detect diacetic acid (now typically called acetoacetic acid), which would have indicated complications of diabetes or possibly starvation. If diacetic acid is present in the urine, the sample turns a purple or burgundy color. But both children’s samples turned a deep green color, a reaction Følling had never seen before. A search of the literature told him that no one had seen this reaction before. Borgny’s children were excreting an unknown substance into their urine.
[The] samples turned a deep green color, a reaction Følling had never seen before. A search of the literature told him that no one had seen this reaction before.
At his self-made laboratory bench Følling set out to identify the substance. After four weeks of trial and error he devised a way to extract, isolate, and purify the unknown material from the children’s urine. He found that his unknown readily reacted with oxygen in the air and so performed his experiments under an inert nitrogen atmosphere in the hunt for his chemical quarry. The spring was turning to summer when, two months and 22 liters of the children’s urine later, Følling concluded that the unknown substance was phenylpyruvic acid, a chemical not normally found in urine.
How many mentally impaired people had this urinary anomaly, he wondered. Using his simple ferric chloride test as a screening tool, Følling checked the urine of 420 patients at institutions around Oslo, finding eight who tested positive for phenylpyruvic acid. Only five months after Borgny’s initial visit he prepared a report on the 10 total cases of this previously unrecognized disease. He termed the condition imbecillitas phenylpyrouvica. Eventually it would come to be called phenylketonuria, or PKU, a disease that affects 1 out of every 15,000 babies in the United States. In his report, he postulated that since the same rare condition tended to affect siblings, this genetic defect was probably recessively inherited.
Diagnosis did not help the Egelands. Dag died a couple of years later, though Liv survived into her forties, living in an institution. Harry died young, while Borgny lived into her eighties, knowing that her struggles eventually benefited other families.
Simple and Striking
A dozen years later British psychiatrist and geneticist Lionel Penrose observed that the test for phenylpyruvic acid in urine “is so simple and striking that the failure of clinicians to observe the reaction until so recently is puzzling, except on the basis of the difficulty of obtaining specimens from subjects of low mental grade.” Still, as Penrose added in his inaugural lecture at University College London, Følling’s discovery inspired a surge of urine testing of mentally deficient patients in institutions, with reports of findings published in succession in the United Kingdom, France, the United States, Switzerland, and Canada. A single neurophysiologist at a mental institution in New York State tested over 8,000 patients in the mid-1930s.

Penrose’s comment is especially striking considering that in 1934 he published a paper on four related patients having a rare, previously unrecognized, recessive form of inherited mental deficiency. After seeing Følling’s paper Penrose went back and tested the urine of the surviving patient from his study. He found phenylpyruvic acid. So Penrose himself was one of the many physicians who “puzzlingly” failed to observe the ferric chloride reaction in the urine of people with PKU!
Why then did Følling succeed where others failed? The simple ferric chloride test was not an unusual one. But there were many simple colorimetric tests he might have chosen. And none of the available tests, including ferric chloride, had ever been associated with mental retardation. Følling had already done two tests for diabetes and kidney trouble. Why do another?
One possible answer is that Følling was sleuthing, and it took his nose as both a doctor and a chemist to solve the puzzle. From his medical training he knew that certain characteristic smells were sometimes associated with disease. Plus he had the added advantage of being an experienced bench chemist familiar with a range of chemical odors. In pondering the children’s scent he would want to test for substances or conditions that could produce distinct smells. And diabetic ketosis is associated with a distinct scent, albeit a sweet one. Following his nose Følling perhaps took an intuitive stab at finding distinct odor-causing compounds and found something unexpected—a previously unrecognized disease. His intuition led to an elegantly simple test for screening large numbers of mentally deficient patients quickly and cheaply. This innovation fueled PKU research for at least the next two decades.
A Cure for Mental Retardation?
As a metabolic expert, Følling immediately recognized that the phenylpyruvic acid in urine was likely connected to a metabolic problem. In his 1934 paper he speculated that PKU was caused by an inherited error in metabolizing an essential amino acid called phenylalanine, which had a chemical structure almost identical to that of phenylpyruvic acid. In turn Penrose seized on Følling’s supposition that PKU was an inborn error of metabolism. If that theory were true, then PKU was an inherited defect of the liver, not the brain, and so might be treated with a phenylalanine-free diet. Granted, this disease was relatively rare, and a successful therapy would only help limited numbers of patients. But the revolutionary idea that a simple diet could treat a form of mental deficiency was irresistible. Penrose rushed to try it.
Following his nose Følling perhaps took an intuitive stab at finding distinct odor-causing compounds and found something unexpected—a previously unrecognized disease.
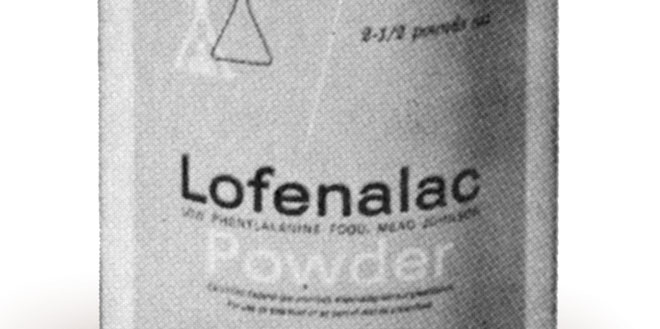
Creating an appropriate meal plan, however, was not simple. As a basic building block of plant and animal proteins, phenylalanine is found in almost all foods. Only water, refined sugar, pure starch, and pure oils are completely free of it. Penrose fed his sole PKU patient—1 out of 500 institutionalized patients he screened with the ferric chloride test—nothing but fruit, sugar, olive oil, and vitamins. Initially, success beckoned when phenylpyruvic acid disappeared from the patient’s urine. Penrose rejoiced, thinking that he saw some improvement in his patient’s mental state. But Penrose’s dietary formula was nutritionally inadequate. After about two weeks phenylpyruvic acid appeared once more in the patient’s urine: lacking dietary protein, the starving patient’s body had begun to metabolize its own protein. The experiment had to be discontinued.
What was needed, Penrose decided, was a protein-replacement formula lacking phenylalanine. He posed the question to Frederick Gowland Hopkins, a Nobel-laureate biochemist at Cambridge University. Hopkins replied that it was possible to create a synthetic phenylalanine-free diet, but the cost would be approximately £1,000 per week, more than many middle-class families earned in a year. Penrose dropped the question.
“She Awaited Me Every Morning”
Ultimately, protein replacement would wait until the end of World War II. During the war years pioneers of PKU research like Følling and George Jervis worked on genetic and biochemical questions rather than therapeutic ones. They worked out the pattern of inheritance, elucidated the metabolic pathway of PKU and where it went awry, created and improved methods of chemical analysis of blood and urine for diagnosis, and looked for biochemical means to identify genetic carriers. Over this period Penrose became convinced that the metabolic anomaly, while always present, did not cause the mental defects seen in PKU patients. Dietary therapy was therefore not worth pursuing in his opinion, and he, too, turned to questions of PKU genetics and carrier detection.
Meanwhile, the two men who would publish the first successful trial of PKU dietary therapy, Horst Bickel and John Gerrard, were serving as medical officers on opposite sides of World War II—Gerrard with the British Army and Bickel with the German Navy. Bickel’s first introduction to PKU took place after the war, while working under famed pediatrician Guido Fanconi in Zurich. PKU’s rarity, and the significant distractions of war, meant that many doctors still knew nothing about the condition. Early one morning in 1949 Fanconi read a report on PKU and during morning rounds surprised Bickel by asking why their mentally deficient patients had not been screened with the ferric chloride test. Bickel had to admit he had never heard of PKU. They immediately began testing their patients for phenylpyruvic acid. After months of screening they found none with the characteristic abnormality, and the ferric chloride bottles disappeared from the shelves. But Bickel would now be watching for it.

Bickel got his opportunity to study PKU firsthand later that year as a new research fellow at the Children’s Hospital in Birmingham, England. Like Zurich, Birmingham turned out to have an excellent pediatrics center. Wanting to impress his new colleague, Gerrard, Bickel asked why they were not screening for PKU in Birmingham. Caught unaware, Gerrard promptly introduced the ferric chloride test to the pediatric ward. They got a positive result on the third child tested, a two-year-old girl named Sheila.
Sheila could not stand, walk, or talk. She showed no interest in food or in the surrounding world and spent her time groaning, crying, and banging her head. She also had the smell, described by Bickel as mouselike. As he later remembered it, Sheila’s mother “was not at all impressed when I showed her proudly my beautiful paper chromatogram with the very strong phenylalanine spot in the urine of her daughter.” The mother wanted more. “She awaited me every morning in front of the laboratory asking me impatiently when I would at last find a way to help Sheila.” The distraught mother would not accept the lack of any known treatment for PKU.
Help came in the person of L. I. Woolf, a chemist at the Hospital for Sick Children, Great Ormond Street, in London. In the aftermath of World War II, Woolf had spent time working on a milk protein called casein, breaking it down into its amino acids for use as a “predigested food” to treat starving people in Europe. Now at the Hospital for Sick Children he encountered PKU for the first time. In addition to his postwar nutritional experience Woolf knew of a method published in 1943 by German chemists for removing phenylalanine from hydrolyzed casein. He realized that this method, passing the amino acid mixture through acid-washed activated charcoal, could produce a phenylalanine-free formula for PKU. Woolf had had no luck in persuading his hospital’s physicians to test this protein replacement on patients with PKU, but Bickel and Gerrard wanted to try it.
The researchers fed Woolf’s formula to Sheila, along with vegetables, fruit, and gluten-free bread and flour. She ate this low-phenylalanine diet for four weeks, during which time the researchers observed that her musty smell disappeared, the levels of phenylalanine in her plasma and urine fell to normal, and she stopped excreting phenylpyruvic acid. But, like Penrose’s PKU patient two decades before, Sheila’s body began to break down its own proteins, creating phenylalanine in the process. Bickel and Gerrard realized that they needed to find the right balance of the amino acid: one that allowed bodily growth but did not allow excess accumulation in the blood. They began to include a daily intake of milk to provide the small amount of phenylalanine needed. After several months on this diet Sheila crawled, stood, and climbed on chairs. Bickel reported that her “eyes became brighter, her hair grew darker, and she no longer banged her head or cried continuously.”
One Disease, Many Lessons
Sheila wasn’t cured, but from these modest beginnings researchers would learn that if administered from birth, this dietary prescription would prevent mental disability. Using work on PKU as a model, support for research in the prevention and treatment of mental disability flourished. Screening programs were gradually established to identify at birth children with PKU, and it became the first of many genetic conditions for which infant screening would eventually become mandatory in the United States.
In the world of science PKU research contributed to biochemical concepts like the existence of metabolic “pathways” and spurred further research on the relationship between genes and proteins. Genetic diseases also took on new meaning; they were no longer seen as inalterable. A new branch of medicine, medical genetics, would concern itself with diagnosis, prevention, and treatment of inherited disorders like PKU.
The protein formula for PKU became the first dietary therapy for a metabolic disease—and the first medical food—becoming a model for the treatment of many other metabolic disorders. Subsequent generations of pediatricians and nutritionists would work on ways to make the highly restrictive diet more tolerable for long-term use and the unpalatable protein formula more acceptable. But crucial early advances in disease discovery and dietary therapy came from chemists, without whose scientific sleuthing and creativity many more children would have grown up needlessly suffering from this preventable form of mental disability.