Research into spinal-cord injuries sometimes seems futile. Over the past century millions of hours of labor and untold millions of research dollars have poured into the field—and all that effort has yielded exactly zero treatments for spinal-cord damage. As one neurologist remarked, “It would be difficult to find any other branch of science with over a century of such sterile endeavor.” But in the past decade those gloomy prospects have brightened considerably, thanks to a simple chemical called PEG.
PEG stands for polyethylene glycol, a long-chain polymer with an incredible thirst for water molecules. It was first created in 1859 and has since been used in a dizzying variety of products, including toothpaste, artificial smoke, and antifreeze. Perhaps most famously, archaeologists have used PEG to protect the fragile paint on China’s terra-cotta warriors from humidity in the air and to preserve the wooden bodies of ancient shipwrecks. In the latter case wooden hulls emerge from the briny deep quite waterlogged, often with the consistency of wet cardboard. PEG stabilizes the wood and replaces the water molecules inside wood cells, which prevents the planks from shrinking and cracking as the wood dries out.
PEG has uses in medicine as well, most commonly as a laxative. As a water-thirsty molecule PEG prevents the intestines from reabsorbing the water in stools, which keeps the stool soft and heavy and makes it easier to pass.
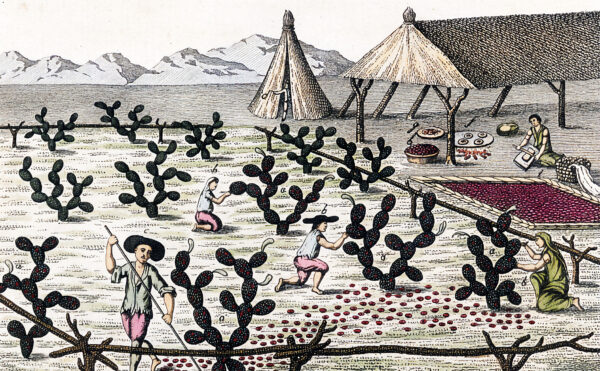
More recently biotech firms have used PEG to create antibodies that fight diseases. Antibodies are normally produced by certain white blood cells, but those cells don’t grow well outside the body, making antibodies hard to mass-produce. Two scientists finally got around that limitation in the 1970s by, of all things, mixing PEG with cancer cells. César Milstein and Georges Köhler knew that cancer cells, however destructive inside the body, grow quite nicely in the lab. So they began looking for ways to fuse antibody-producing cells with cancer cells to take advantage of the good traits of both. After a failed attempt using viruses Milstein and Köhler succeeded in creating these “hybridomas” with PEG. The polymer seems to promote the fusion of cells by dehydrating and breaking down their membranes, forcing the cells into close contact and allowing them to glom together. Milstein and Köhler’s work on antibody production won them a Nobel Prize in 1984 and helped spawn a multibillion-dollar industry that has produced treatments for Crohn’s disease, rheumatoid arthritis, several types of cancer, and immune rejections in transplant surgery.
PEG’s ability to fuse cells also explains why the polymer shows such promise in treating spinal-cord damage. Nerves outside the spinal cord—which carry signals to your limbs and organs—can regrow, albeit slowly, after they suffer damage. Nerve tissue inside the spinal cord doesn’t regrow after damage, meaning that spinal-cord injuries usually cause permanent paralysis.
But PEG could get around that limitation. When applied to damaged spinal cells, it breaks down their membranes and allows the cells above and below the injury site to fuse together. As a result, signals from the brain—which once fizzled out at the gap—can now cross the site of the injury and connect the brain and lower body once again.
So far PEG has proven effective in treating spinal-cord paralysis in a variety of mammals, including dogs. I personally witnessed the magic of PEG in mice while visiting a research lab in China. There I watched two graduate students surgically sever the spinal cords of several mice, which should have rendered their hind legs useless. (They cut the cords halfway down the back.) But before sewing up the mice, the students squirted in a few drops of PEG dissolved in water, a solution with a faintly amber color. Two days later these mice were walking again. Not perfectly: they still lurched somewhat. But compared with control mice—who received no PEG, and who were dragging their dead back legs behind them—the PEG mice had made a near-miraculous recovery.
Right now PEG remains experimental. Success in lab animals doesn’t guarantee success in human beings, and no one knows how well PEG—which in the lab usually gets applied immediately after spinal damage—would work on long-standing injuries, which are often covered with scar tissue. (Surgeons could perhaps get around this by making fresh cuts that pare the scars back.) But PEG and other chemicals that fuse cells (collectively called fusogens) do show genuine promise. In the United States alone, 11,000 people suffer spinal-cord damage each year, with no prospects for improvement. After a century of such sterile endeavor, even a modest sprig of hope is worth celebrating.