When I walked in, I saw my father surrounded by medical devices, each beeping or humming as it gathered information about his condition. The nurse who walked in with me pointed at the clear plastic bottle hanging on the wall and said, “You can tell he’s dehydrated. Look at how dark and thick his urine is.”
I was struck by the nurse’s apparent preference for an old-fashioned and simple diagnostic over the sophisticated and surely expensive medical gadgetry that filled the room. Her comments would have been equally at home in a bedroom in the 15th century or an alchemist’s library in the 17th. For centuries medical practitioners relied on urine as a diagnostic tool, evaluating the color, the cloudiness, the thickness, the smell, and even, so we read, the taste. And despite the development of analytical tests that quantify urine’s specific gravity and concentration of glucose, measure its pH, or detect the presence of foreign substances, visual inspection remains a common diagnostic technique both for health care providers and for the average person browsing the web.
Medicine today shares almost nothing with the early modern period, so how do we explain the persistence of uroscopy?
Early modern physicians paid special attention to urine’s consistency and color. Urine was categorized as thick, ordinary, or thin. We are left to wonder what distinguished thick from thin, and early modern authors offer little clarity. In some cases, the intensity of color seems to have been a factor. Thick urine might be the same color as thin, but it would appear darker. According to one rule of thumb, if the physician could not see his finger joints when looking through a flask of urine, it was considered thick. In other cases, physicians relied on sound, the noise it made when poured into a container of water. When poured from a comparable height, healthy urine and good wine made the same sound. Let’s applaud the early modern physicians who could distinguish between the sound of good and bad wine.
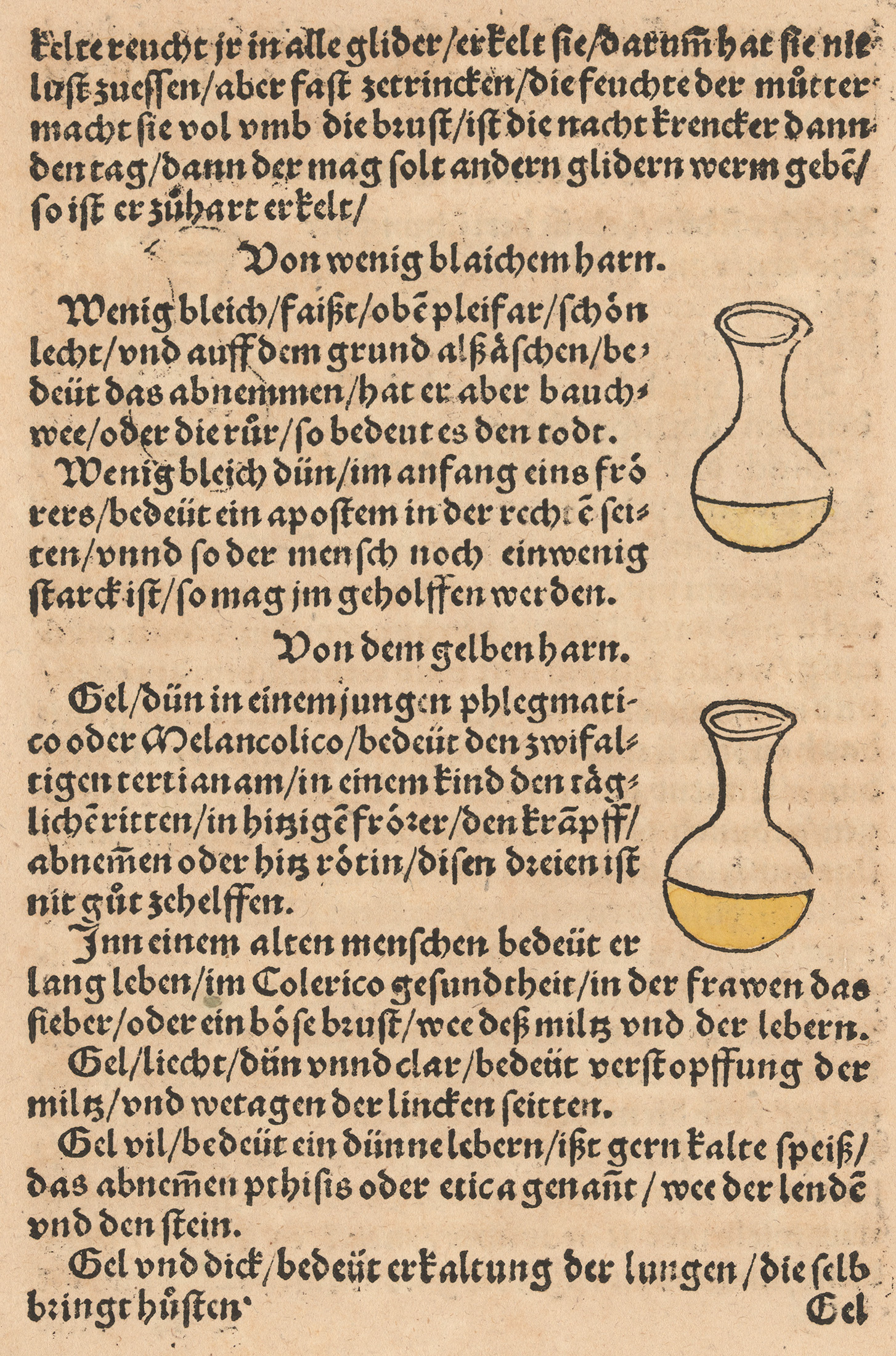
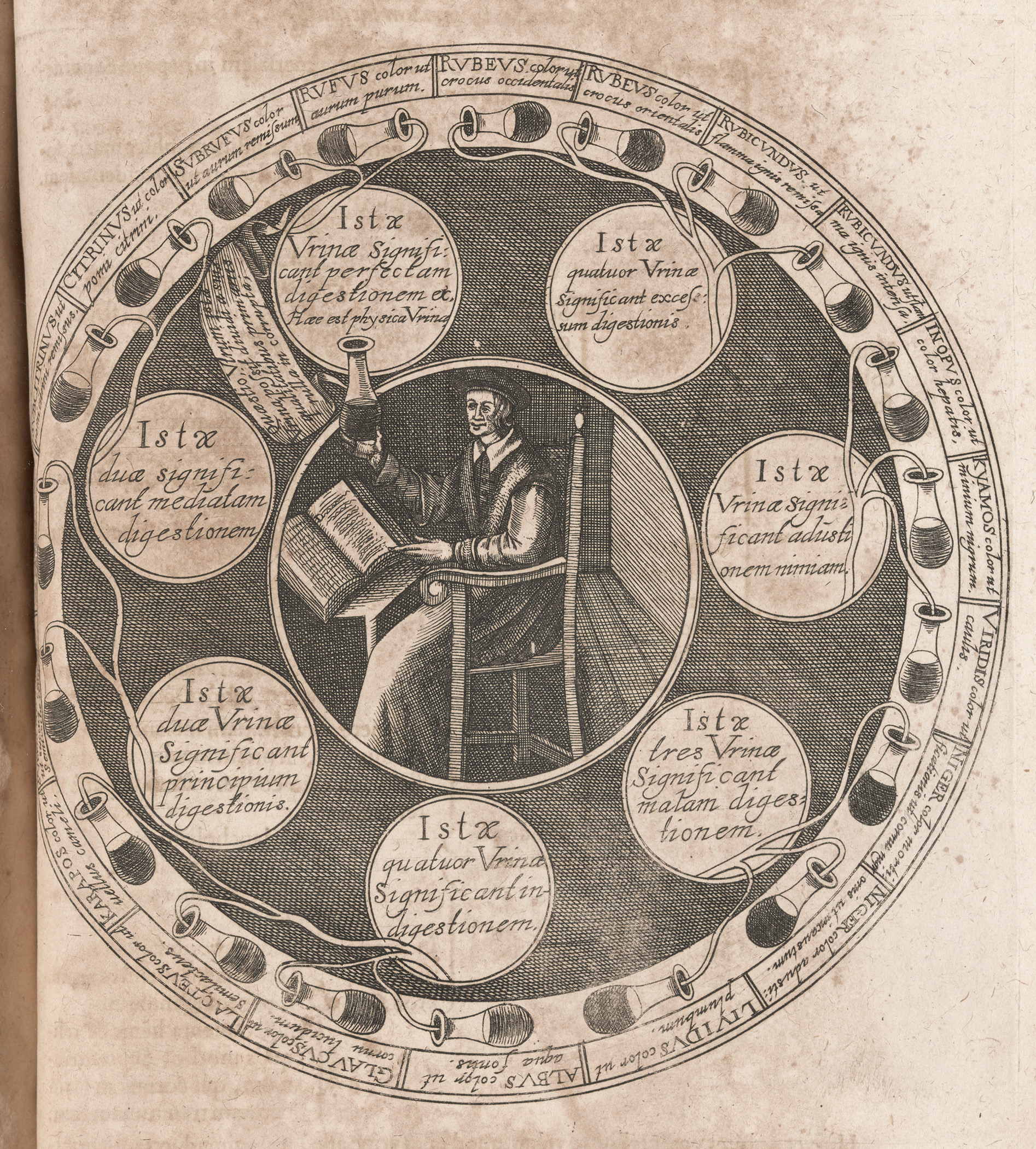
Color, however, was more important than consistency. In medical manuscripts we find a sort of color wheel of urines, depicting up to 20 urine-filled flasks of different hues and shades. Each flask was colored and typically labeled with some common liquid or object as reference along with a brief description of the color’s associated illnesses. Thin blue urine could indicate a patient suffering from excess melancholy and a severe cold. Very red, almost bloody, urine could indicate disease in the kidneys. Diagnosis often took into account whether a patient was a man or woman. For example, in women reddish urine often indicated pregnancy or lovesickness. In one case, however, a physician diagnosed a woman with an inflammation of the liver based on her “reddish” urine.
Although uroscopy was grounded in a shared medical theory stretching back to antiquity, these early manuscripts were often idiosyncratic, reflecting local experience. Colors and the corresponding diseases varied considerably between texts.
With the spread of printing, texts on uroscopy became more widely available. But print introduced a new issue. Because ink was either black or, in limited cases, red, color wheels of urine in printed books lacked actual color. Some owners, worried about this obvious limitation, hand colored the flasks to match the descriptions. However, those descriptions themselves were often unhelpful in picking out an appropriate color. For example, we find subcitrinus and citrinus both described as the color of a yellow apple, the former labeled “fully yellow,” whatever “fully yellow” might mean. In another example, one flask is described as “white as gold,” while the next is labeled “red as gold.” Owners seemed to have thrown up their hands, using whatever colors they had lying around to tint the flasks. Unsurprisingly, then, we find little consistency between copies in colors used for the flasks, no obvious correlation between the description and the color used, and frequent reuse of the same color for different descriptions.
In the 17th century, physicians proposed weighing urine to quantify its contents as part of a broader effort to establish a chemical basis for medicine. Jan Baptist van Helmont, for example, weighed urine samples and compared them to an equal volume of rainwater. He found that the samples varied widely: a healthy 35-year-old woman’s urine weighed 75 grans more than rainwater. He also measured urine in two healthy 19-year-old men; he found one had urine 1130 grans heavier than rainwater, while the other’s was 4 grans lighter than rainwater. Later, when the second man was suffering from a fever, he excreted urine that weighed 178 grans more than rainwater. In another case, a young woman with a heart tremor produced urine that weighed the same as rainwater. Van Helmont did not speculate about what actually caused the differences in weight and, in the end, gave up.
Weighing urine found little support until well into the 18th century. In 1756 Johann Friedrich Rübel published Medicinische Abhandlung, the results of his research on sicknesses, and included a chapter on urine. He assumed urine contained dissolved substances that increased its weight and tried to determine a normal range for that weight. For two weeks he meticulously recorded what he ate and drank while he collected and weighed a fixed volume of his urine. His results, like van Helmont’s, varied too much to establish a normal range. When weighing the urine of sick patients, Rübel found that patients suffering from uterine pain, spleen or stomach complaints, cramps, stones, and gout, as well as headaches, dizziness, mania, fever, madness, falling sickness, or nervous diseases, all excreted urine that was lighter than expected. Weight, it turned out, offered little diagnostic value beyond confirming that somebody was sick. Nonetheless, he remained confident that “the science of urine and urine examination [had] no small role in medical practice.”
Scientists in the 19th century seemed to heed Rübel’s urging by developing a range of tests and devices to analyze urine. Early in the century they created the urinometer to determine the specific gravity of urine, a device primarily used to tell whether a person suffered from diabetes. The physician filled a vessel with the patient’s urine and then floated a weighted bulb in the urine. A graduated scale sticking out of the top of the bulb allowed the physician to determine how low in the urine the bulb sank. The scale on early urinometers was marked with “W” for water, “H” for healthy, “S” for strong but likely fighting something, and “Diabetes.” Another device, the albuminometer, quantified the amount of albumin in a urine sample as a measure of how well the kidneys were functioning. Microscopy allowed physicians to examine sediments, bacteria, and other particles in a sample. These 19th-century analytical techniques promised to replace uroscopy with urinalysis. An overly ambitious promise, as it turns out.
Despite the proliferation of analytical techniques with their quantified results, physicians continued to rely on the qualitative, visual inspection of urine. For example, the Somogyi method, developed in the first half of the 20th century, was a qualitative technique to screen for diabetes. The A.S. Aloe Company developed “urine sugar comparator” devices that made using the Somogyi method convenient. The physician would match a patient’s urine sample to one of a series of colored standards on the device, each of which corresponded to a specific concentration of glucose.

A.S. Aloe also developed strictly quantifiable tests. One was the Squibb urinometer, which like earlier urinometers determined the specific gravity of urine as a measure of the amount of glucose in a sample. On this version of the urinometer, numbers replaced the lettering on earlier devices, but it otherwise functioned the same. Specific gravity that fell outside a normal range might suggest diabetes, but the number needed to be supplemented by visually inspecting the urine sample, as an early 20th-century textbook makes clear.
Published in 1927, Lotta Jean Bogert’s Fundamentals of Chemistry and the accompanying Chemical Laboratory Manual, both intended for nurses, illustrate how qualitative and quantitative techniques went hand in hand. In the lab manual, Experiment 88, “Normal Urine,” instructs the student first to note the color and appearance of a urine sample, then to use litmus paper to determine acidity, and finally to measure the specific gravity. A corresponding table in the textbook reveals what abnormal-looking urine might mean: a greenish-brown color is the result of bile in the urine; reddish “may be due to blood or foreign pigments”; milky is caused by pus or fat. The next row of the table gives the normal range for specific gravity, 1.010 to 1.030. But even here visual inspection continues to play a role: a high specific gravity is “usually due to sugar in urine (diabetes mellitus), if associated with large volume and light color.” The textbook leaves it to the student to decide what is and is not “light color.”
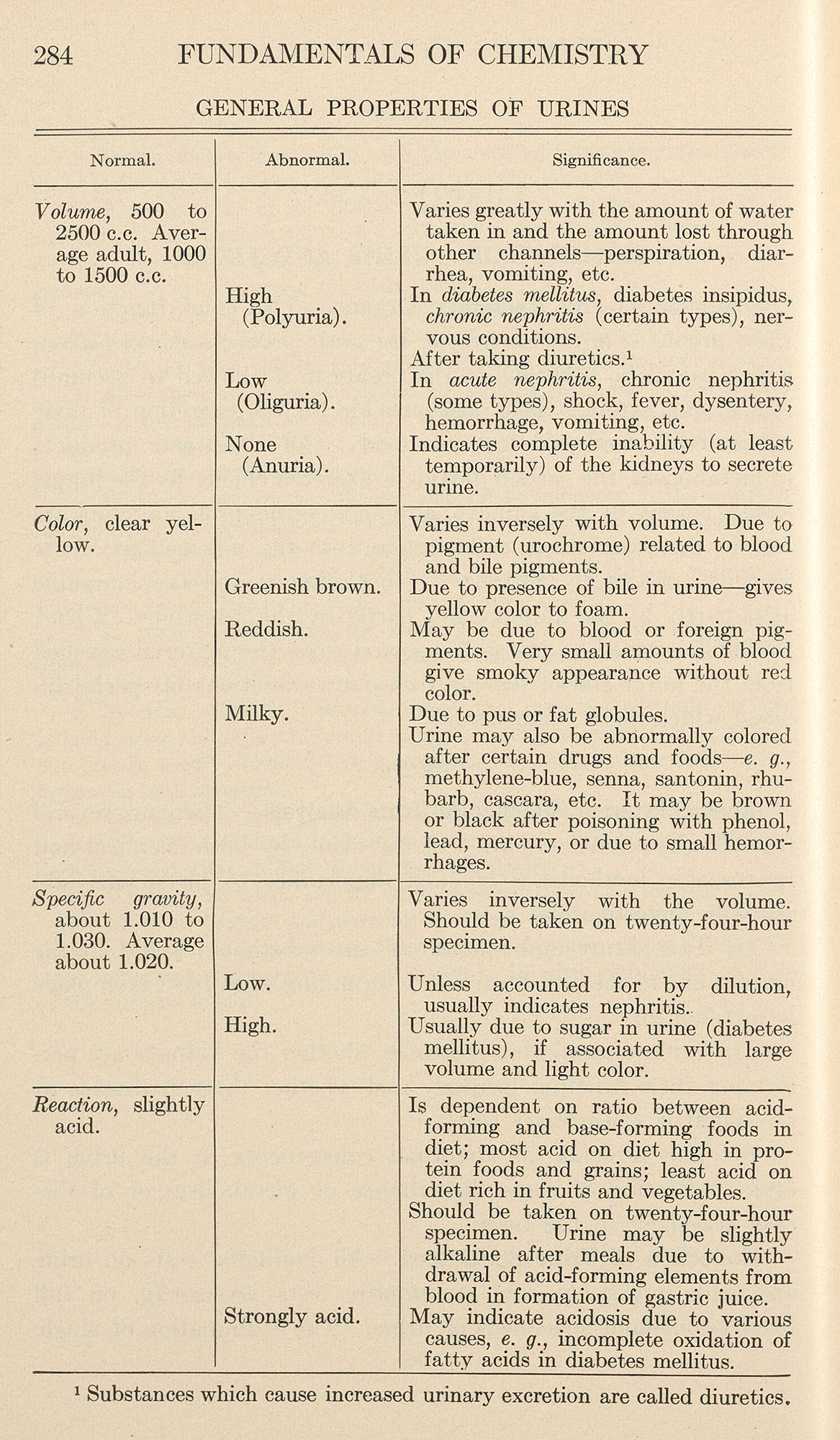
Today’s medical textbooks and manuals still include a chapter on uroscopy, masquerading as analysis. Chapters with titles like “Physical Examination of Urine” or “The Routine Examination of Urine” open by describing the range of colors of normal urine in vague terms: “pale to dark yellow,” “pale yellow to amber,” or “almost colorless to black.” Some of these “normal” colors, such as black or pink-red, could be temporary conditions arising from medications or diet. The colors of abnormal urine, similarly, vary considerably and often overlap with those of normal urine. Tables correlate colors with possible causes, both pathological and nonpathological: white could be caused by excessive lipids and fats, or just vaginal cream; amber indicates an excess of bilirubin and possible liver problems, or too many carrots in your diet; a “port wine” appearance indicates porphyria, but should not be confused with red-brown, which is caused by myoglobin.
The first column of these tables offers a bewildering range of overlapping colors: milky, pale yellow, dark yellow, yellow-orange, orange-yellow, yellow-brown, yellow-green, pink to red, red to purple, brown to black. Turning to the column of causes, I begin to think the chromatic precision suggested by the first column is something of a charade. Often a condition reoccurs as a cause for a number of different colors (e.g., bilirubin might cause yellow-orange, yellow-green, yellow-brown, or brown to black urine). Deciding which color best describes a urine sample and distinguishing between possible colors is left to the expert eye of the physician.
Two such experts, neuroscientists and podcasters Dr. Matt and Dr. Mike, recount this challenge in a 2021 episode, “Urinalysis—What is in your wee?” The doctors devote the opening segment to the color of urine and what it could indicate about the patient’s health, justifying this focus by saying that it is “important to probably highlight the fact that . . . before you can do these specific tests [e.g., test the pH or specific gravity], you can actually just look . . . to see what the urine may look . . . like to give some more clues and hints.”
They largely recapitulate the tables found in textbooks: normal urine is straw colored and suggests the patient is hydrated. Darker yellow is dehydration. Red or pink could indicate some blood in the urine, or certain drugs, or maybe just particular foods. Brown, distinct from amber, could be indicative of myoglobin or other proteins. In the end, they admit that different foods, drugs, proteins, and even bacteria could affect the color of urine.
Given the uncertainty in their discussion, the importance of looking at urine must be more than the “clues and hints” the physician might glean from the urine’s color. I suspect the importance has more to do with the act of looking at the urine, how it conveys an image of expert knowledge.
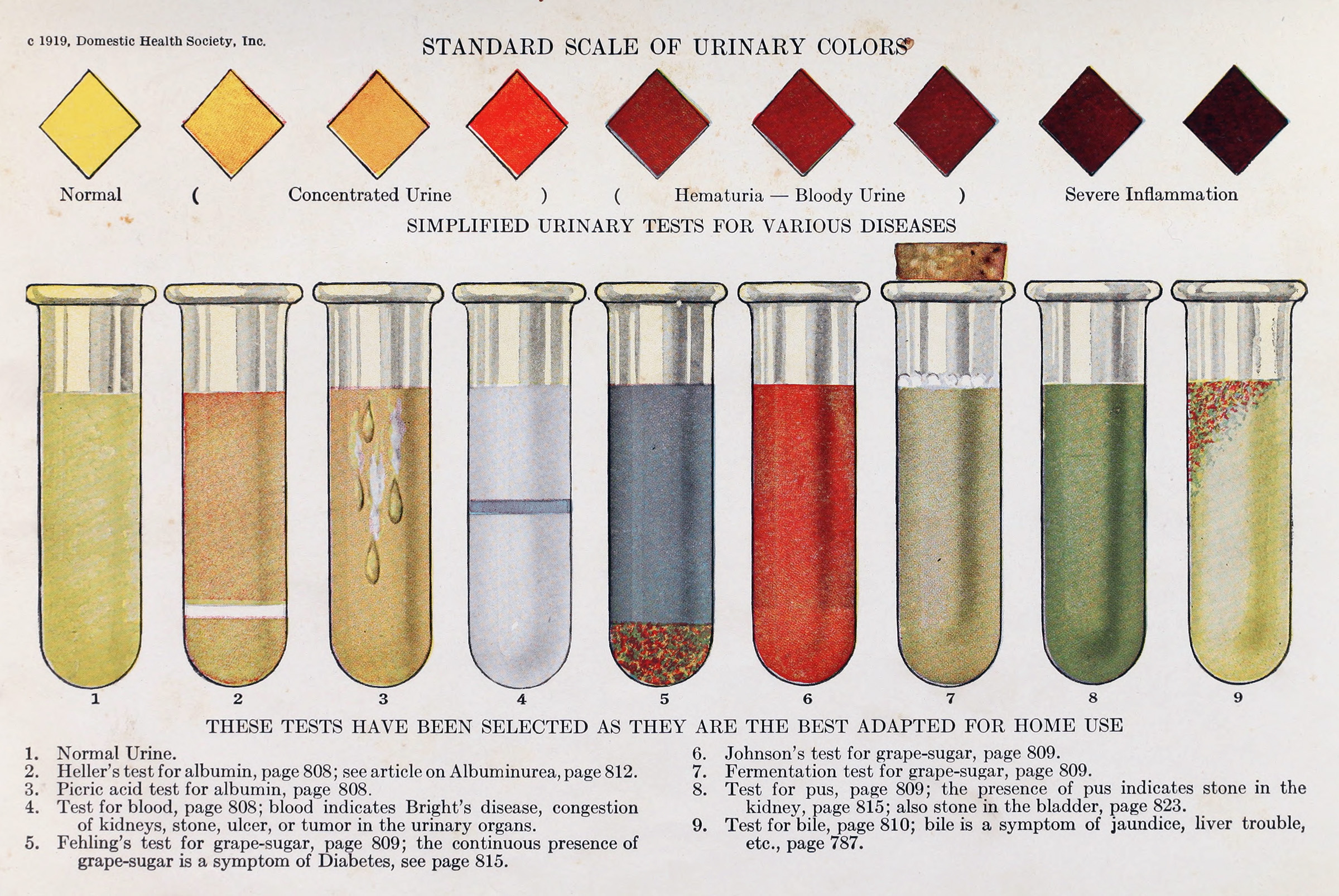
Uroscopy is so common that it has become a rule of thumb for self-diagnosis. Reputable medical institutions, such as the University of California, Irvine, and the Cleveland Clinic, post articles with titles that at times seem to echo language more commonly found in pop-psychology articles—“What Your Urine’s Color Means” and “What the Color of Your Pee Says About You.” Color charts invite visitors to guess what color best matches their own urine and then infer what might be ailing them.
Online urine color charts abound. These charts often use colloquial language that is at once oddly precise and yet still ambiguous, while encouraging visitors to self-diagnose and even treat their conditions. Is your urine honey color? “It’s nothing to worry about, but drink some water.” Does your urine resemble lemonade (but not light beer)? “This is optimal hydration. Keep doin’ what you’re doin’.” Is it burnt orange? “Drink lots of water and electrolytes.” For more unusual colors, these charts offer ominous predictions: green or blue is “usually a result of a rare genetic disease”—or maybe food dye.
And here is the key: underlying these articles and charts, as well as the tables in urinalysis textbooks, is a sense that urine is too nuanced and subtle for the untrained layperson to understand. Normal color is ambiguous and context dependent, and there are overlapping and contradictory causes for both normal and unusual colors. Only trained medical professionals have the knowledge and expertise to read the color as a sign that everything is OK or that something has gone horribly wrong.
Despite the many developments in modern science and medicine, I should not have been surprised by the nurse’s initial comment about my father’s urine and what it told her. Uroscopy is thriving today, doing what it has always done: giving physicians and nurses the chance to perform a type of expertise that encompasses the patient’s health. Or, put another way, looking at urine resembles a form of divination. The patient and physician both see something, maybe a clear bottle filled with yellowish liquid hanging on a wall. The patient would agree that it is a bottle of pee but usually does not have the knowledge to say much more. For the person who has mastered a body of esoteric knowledge and wears a special outfit to prove it, that bottle of urine is rich in significance, an opportunity to reveal hidden layers of meaning and a chance to glimpse at what could be happening inside the patient and therefore what the patient might soon suffer.
This morning my pee is a surprisingly strong, bright yellow with an unmistakable tinge of green. I would say, brighter than “lemonade,” not as neon as a “highlighter,” but somewhere in that “yellow-to-green” range. According to a recent textbook, it could be bilirubin oxidized to biliverdin. Online charts suggest I might have too much vitamin B in my system or I might not be sufficiently hydrated. One encourages me to seek medical advice if the condition persists. My guess is, however, the cause is nothing more exotic than last night’s asparagus.