When an allergic reaction to a drug or a food hits, or when an insect bites or stings, you or someone you know may reach for an EpiPen. A quick jab into the outer thigh activates a spring-loaded plunger, a hollow needle is pushed into the muscle, and epinephrine is released. Without epinephrine someone at risk for anaphylactic shock can die from a significant drop in blood pressure as blood drains from vital organs, such as the heart and brain, or from swelling that shuts off airways.
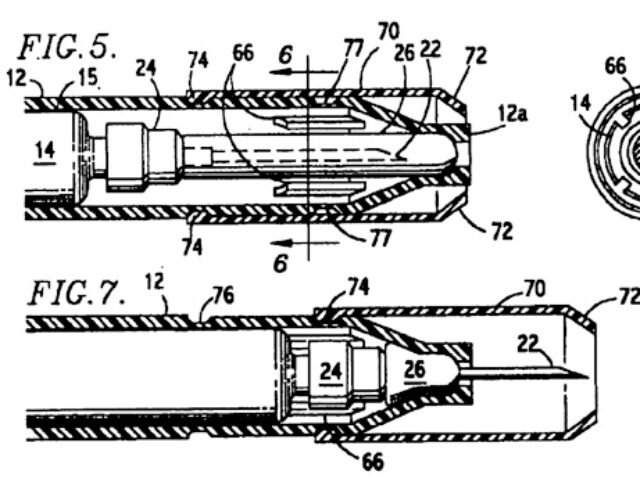
EpiPen is the more commonly used trade name for an epinephrine autoinjector. No bigger than a cigar, the device is a Cold War spin-off based on the 19th-century innovation of hollow-needle injections. During the Cold War the military wanted a quick way for troops to self-inject antidotes to nerve gas. In the 1970s inventor Sheldon Kaplan recognized that modifications in the pen could turn it into a lifesaver for civilians, especially those susceptible to anaphylactic shock, where a fast response can mean the difference between life and death.
The EpiPen gradually replaced a World War II innovation, the Ana-Kit, which contained measured doses of epinephrine ready to be delivered by syringe and needle. Before World War II, treatment required drawing up and measuring epinephrine from a vial, a time-consuming and error-prone method.
Epinephrine—also known as adrenaline—is a hormone. Both words mean “atop the kidneys.” The substance was discovered in the 1890s after Englishman George Oliver began experimenting with extracts from various animal glands. One extract from the inner part of the adrenal gland increased the blood pressure of a dog. Almost as soon as it was discovered, physicians and pharmaceutical entrepreneurs began seeking uses for this substance.
Among these entrepreneurs Philadelphia’s Solomon Solis-Cohen has been credited with being the first to try epinephrine on patients diagnosed with hay fever and certain types of asthma. In 1898 Solis-Cohen tried “suprarenalin substance” prepared from sheep adrenals by a local pharmacist as a palliative for his own and his brother’s relatively mild seasonal hay fever. Solis-Cohen thought hay fever was ultimately caused by a weakness of the nerves and muscles controlling the dilation and constriction of blood vessels and was “perhaps aggravated by a somewhat studious life.” The epinephrine helped but not for the reasons Solis-Cohen expected. Later research showed his successes were primarily due to epinephrine’s relaxing effect on the smooth muscles lining the airways.
By 1900 Solis-Cohen had begun to use an adrenal substance to treat patients with some types of asthma, a condition then still being defined. He gave his patients tablets but complained about the unnecessary animal substances they contained that could cause diarrhea. He joined the hue and cry for purity. “If we could have the active agent alone, our therapy would be much more definite.”
In a 1906 article Solis-Cohen named the scientists who responded to this need. He described using “both the adrenalin chloride solution of Takamine and the epinephrine of Abel,” the latter marketed as a powder—Suprarenalin—that could be made into tablets. Only at the very end of Solis-Cohen’s article, when he describes what to do should these fail and “asthmatic paroxysms” occur, does he mention injection as the quickest way of applying the drugs.
John Jacob Abel and Jokichi Takamine were both working in the United States at that time. Abel was Johns Hopkins Medical School’s first professor of pharmacology. In 1897, by using various separation techniques, he managed to obtain a crystalline product from sheep adrenal glands, which he called epinephrine. He had not, however, isolated the pure substance but probably a slightly impure derivative of it. (Today’s EpiPen contains laboratory-synthesized epinephrine.)
Takamine was a chemist with an entrepreneurial bent who had been educated in his native Japan and in Scotland. By 1900, when Takamine began adrenaline (his term) research in his Clifton, New Jersey, laboratory, he had already isolated enzymes from Aspergillus oryzae—a fungus essential in producing soy sauce and miso—and patented the product as Taka-Diastase, an indigestion remedy. He sold the patent to Parke-Davis and Company, a Detroit pharmaceutical firm. Similarly, when he and his assistant succeeded in purifying epinephrine, Takamine sold these patents to Parke-Davis, which trademarked the product as Adrenalin.
Starting in the late 1960s, researchers Robert J. Lefkowitz and Brian K. Kobilka worked to identify the receptor molecules in cell walls that link with epinephrine molecules to trigger various physiological responses, such as elevated blood pressure. For discovering where and how epinephrine works in the body, the two men received the 2012 Nobel Prize in Chemistry.
Over the years epinephrine has been used to treat mild asthma and allergies and as a means of restarting stopped hearts. Today its only official use is in treating anaphylactic shock—when a body needs a lot of its systems restored in a hurry.