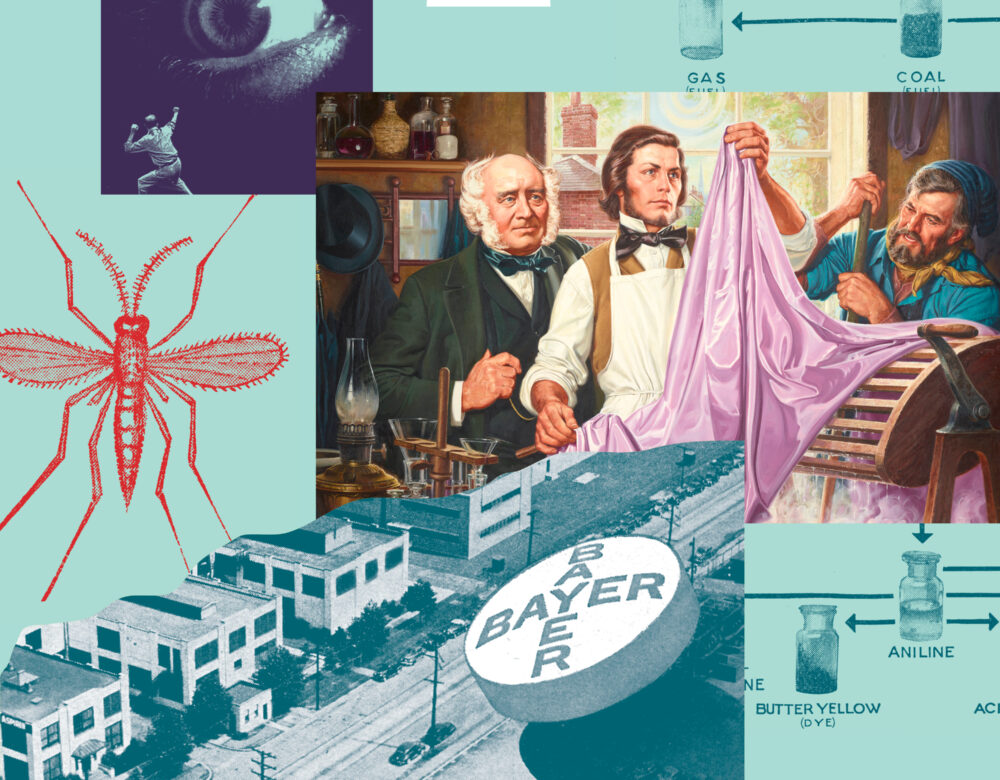
In 1856, Henry Perkin’s attempt to synthesize quinine led to something very different: a vibrant purple dye. Perkin’s mauve revolutionized the fashion industry when Queen Victoria wore a dress of the color to her daughter’s wedding. And in an ironic twist, synthetic fabric dyes ultimately led to synthetic drugs, including the first antipsychotic. This drug, known by its trade name Thorazine, was a game changer. “Nobody thought there could be a drug that would treat schizophrenia effectively,” says sociologist Andrew Scull, “and then suddenly there was.”
In this episode we explore the enduring relationship between dyes and drugs, and the role that mistakes and serendipity still play in drug development.
This episode was inspired by our museum exhibition, BOLD: Color from Test Tube to Textile, on view through August 3, 2024.
Credits
Host: Alexis Pedrick
Senior Producer: Mariel Carr
Producer: Rigoberto Hernandez
Associate Producer: Sarah Kaplan
Audio Engineer: Jonathan Pfeffer
“Color Theme” composed by Jonathan Pfeffer. Additional music by Blue Dot Sessions
Resource List
We, the mentally ill from Smith, Kline & French Laboratories
Mauve: How One Man Invented a Color That Changed the World, by Simon Garfield
The Curious History of Medicines in Psychiatry, by Wallace Mendelson
Molecules, Madness, and Malaria: How Victorian fabric dyes evolved into modern medicines for mental illness and infectious disease, by Wallace Mendelson
Desperate Remedies: Psychiatry’s Turbulent Quest to Cure Mental Illness, by Andrew Scull
Criminal at large from Office of Malaria Control in War Areas
“Conversation between Salvador Dali and Professor Henri Laborit” from National Office of French Television Broadcasting
“Psychiatric Survivor Protest Outside of Smith, Kline and French Office”
Transcript
Alexis Pedrick: In 1955, NBC aired a TV special called “We, the Mentally Ill.” It was part of a series sponsored by the American Medical Association and the pharmaceutical company Smith, Kline and French. In an unprecedented move, patients themselves hosted the TV program.
We, the Mentally Ill: I am a mental patient at St. Elizabeth’s Hospital in Washington, D. C.
For ages, people like us have been hidden in darkness. Now you can see me, and in a moment you will see others like me. You’ll learn from us the conditions of our hospitals today, how mental patients used to be treated, that you can better understand the present by understanding the past.
Alexis Pedrick: In 1955, there were more than half a million patients in US asylums. Overcrowding was a huge problem, but it was also the norm. There were too many patients with too few doctors or nurses to treat them.
And there wasn’t a lot of hope that any treatments would even be effective.
This is sociologist Andrew Scull, the author of “Desperate Remedies, Psychiatry’s Turbulent Quest to Cure Mental Illness.”
Andrew Scull: So over time, simple arithmetic tells you that a larger and larger fraction of an asylum’s population were chronic patients. And that became the asylum’s image. And it became obvious that once you didn’t get out in the first year or 18 months, you probably weren’t going to get out except in a pine box.
Alexis Pedrick: Back in the TV special, we’re introduced to a patient named Sally. She reclines on a hospital bed, her dark curly hair is a bit messy, and she’s leaning back against the pillows, wearing a slightly rumpled house dress. A doctor in a white lab coat sits at the foot of the bed asking her questions.
We, the Mentally Ill: It says over here that you hear voices. What do they say to you?
Alexis Pedrick: She responds, but not to the doctor. It’s like she’s having a conversation with someone who isn’t there.
We, the Mentally Ill: What do the voices say to you?
Alexis Pedrick: Sally seems disoriented. In the next shot, she doesn’t speak. Instead, she holds her hand up to the camera as if to say, stop, and she shakes her head no. Then she presses one finger over each eye, holding them shut, and shakes her head again. Then we hear Sally’s voice, clear and calm, narrating over the scene.
We, the Mentally Ill: This is me when I came to the hospital. I was very upset from many worries. They make me sick. I could not even talk to the doctor.
This is me four days later. After the doctor gave me some medicine to help me. Now I’m not so mixed up. I talk to him okay.
Alexis Pedrick: In the next shot, we see Sally sitting in the doctor’s office. And she looks like a completely different person. She’s wearing a blouse, her hair is combed, and she’s wearing makeup.
We, the Mentally Ill: How would you compare your condition today, let’s say, to the way it was when you first came here? Do you remember how you were when you first came here? What’s the difference? Well, I was, I know it was something in my nerves, maybe, because I tried to help, but I can’t help it. What did you feel then that you don’t feel now?
I feel like, um, I talk just to myself. I don’t feel like talking to nobody else. Just to myself.
Alexis Pedrick: In the final shot, we see Sally on the street, through the window of the doctor’s office. She turns and waves goodbye to him.
We, the Mentally Ill: I say goodbye to my doctor, and I go to see my children again and my husband. I am very happy to go home.
Alexis Pedrick: Then Sally’s doctor turns and talks directly to the camera.
We, the Mentally Ill: Sally is going home today. Result of treatment with new drugs and psychiatry. Drugs that were not even available as much as two years ago. Their names are Chlorpromazine and Rauwolfia. These new medicines have effected a tremendous change in all the psychiatric treatment. As a result of their use, patients who were hitherto unmanageable or untreatable or who had resisted all other forms of treatment now have been helped. These drugs have given American medicine the greatest opportunity of its age to reduce the huge burden of mental illness that falls upon us all. And so you’ve heard from mental patients themselves and those who are trying to help them.
Of the crowded conditions and the shortage of staff. But suddenly now, there is new hope for all. For you, the public, who pay the bills. And for us, the mentally sick.
Alexis Pedrick: In 1954, just one year before this TV special aired, Smith, Kline and French had brought the drug Chlorpromazine to market. Better known by its trade name, Thorazine, it was the very first anti psychotic drug. Actually, it was the very first drug that treated any mental illness.
Andrew Scull: Nobody thought there could be a drug that would treat schizophrenia effectively, and then suddenly there was.
Alexis Pedrick: Thorazine was a game changer. It was initially marketed as a chemical lobotomy, which was fitting because one of the treatments it replaced was the actual lobotomy.
So, how did we get this miracle drug? Maybe a scientist had a hypothesis about what caused schizophrenia. That’s what we assume Sally and a lot of the asylum patients were diagnosed with. And maybe the scientist worked tirelessly to find a drug that would treat everyone. It’s a tidy scenario. But actually, science is messier than this.
It’s often literally built off of a bunch of mistakes. So, we’re going on a roundabout journey that took over a hundred years and involved a lot of failures, with a bunch of people who weren’t even thinking about mental illness.
Alexis Pedrick: From the Science History Institute, I’m Alexis Pedrick, and this is Distillations.
Chapter One. Perkins Mauve.
To go to the very beginning of Thorazine’s story, we have to cross the Atlantic and go back to the mid 1800s, when Europe was in the throes of colonizing the globe, and a tiny insect was standing in its way.
NLM Criminal at Large: This is the legend of a soldier and his girl, of his family, of the town he was born in, and of the death that flies by night, the small singing death.
The Anopheles mosquito, bearer of the plague of malaria.
Simon Garfield: So we had all our massive empire out in India and Africa and everyone, and these pale old Englishmen, or pale young Englishmen, were all dying of malaria.
Alexis Pedrick: This is author Simon Garfield.
Simon Garfield: So this was a real issue, and quinine was found to help.
Alexis Pedrick: Quinine, or quinine, as we Americans say it, was an invaluable remedy for malaria.
It comes from the bark of the cinchona tree, which is native to the Andes Mountains in South America. Now, even though there’s no malaria there, indigenous people used the bark to help them bring down other kinds of fevers. This is Wallace Mendelson, a psychiatrist and author.
Wallace Mendelson: The 17th century Spanish missionaries saw the Amerindians using the bark and tried bringing it the downslope to where malaria was so common, and it was found to be very helpful.
Alexis Pedrick: That’s right. The colonizers saved themselves with the plants of the people they were colonizing so they could stay healthy and keep colonizing them. But I digress, they still had a problem.
Simon Garfield: It, uh, came from, you know, the bark of a tree and was expensive and it was quite rare. So if you could make it in a lab, what a fantastic thing.
Alexis Pedrick: Make it in a lab. That would be fantastic. And for the first time, maybe even possible. Chemistry was on the cusp of changing. By the mid 19th century, chemists had a better understanding of the building blocks of nature. And now, they wanted to copy those building blocks in the lab so they could make things like quinine without having to spend a lot of money or travel long distances to get them.
And because this was the Industrial Revolution, the timing was perfect. A very promising building block was lying around everywhere in the form of coal.
Simon Garfield: One of the residues of coal used for, um, for gas was this kind of horrible sludge, um, that you could purchase for no money at all in barrels, because it was just seen as kind of horrible waste.
Alexis Pedrick: It was called coal tar, and it was the first large industrial waste. But where others saw trash, one man saw treasure. That man was the first director of the Royal College of Chemistry, a German chemist named August Wilhelm von Hofmann.
Wallace Mendelson: He believed that coal tar, which actually contains something like 10,000 different chemicals, could be a source for useful products.
Alexis Pedrick: He’d already studied one of the heavier components, creosote, which is still used as a wood preservative. But there was a whole world of lighter compounds which had never been looked at, and he was determined to study them. He’d figured out that quinine was in the chemical class known as amines, which is a nitrogen base.
Wallace Mendelson: And he also intuited that the general shape of quinine was similar to the shape of the coal tar product, naphtha.
Alexis Pedrick: And so, he thought it might be possible to convert naphtha to a synthetic quinine. And he assigned this experiment to one of his most promising students over Easter break. His name was William Henry Perkin, and he was just 18 years old.
Simon Garfield: So he went to his home in the east end of London, and he went to his attic lab, which was probably a very, very dangerous place to be. There was probably no ventilation and, um, I don’t think things like health and safety didn’t really exist. And he was messing around with his quinine experiments and found that he got the molecular structure wrong.
Alexis Pedrick: Did you hear that? He got it wrong. Bad for malaria. Bad for the British Empire. But Perkin saw a bright side, a literal bright side.
Simon Garfield: It produced this purple dye. And he thought, ok, I’ve gone wrong on one sort of experiment, but I found this other extraordinary thing, this color, which previously was only available if you went to the Mediterranean shore and put a million mollusks in bags and somehow found their property, which was a dye and, and hence you could, you could get like a royal purple, which is very, very rare and very expensive.
Alexis Pedrick: Sometimes genius requires tunnel vision. But sometimes, it requires the opposite. The ability to not only learn from your failures, but to see your failures as accidental successes. And this accidental success was just one of many on the unintentional path to Thorazine. Because failure is a huge part of science.
Simon Garfield: His genius, in a way, was realizing that he could make this purple, which he called mauve, he could make it consistently, and he could make it cheaply. And he realized that he could probably get quite wealthy doing this.
Alexis Pedrick: There’d been a growing debate about the field of chemistry in England. Should it be about pure discovery?
Or should it be more practical, something you could bottle and sell? August Hofmann was in the pure discovery camp, and then his star student went home and made something that might as well have slapped him in the face for how frivolous he thought it was. Perkin had crossed a line.
Simon Garfield: He was frowned upon by not only fellow chemists, who thought, oh, you know, hang on a minute, we have to be a bit more ivory tower about our lives.
It’s not about making money at all. It’s about discovery.
Alexis Pedrick: Instead, Perkin made the world a brighter, gaudier place and got rich while doing it. Perkin’s mauve was a beautiful, lavish purple. Not too dark, not too light. It was sort of like if eggplant and fuchsia had a baby. And it really took off when a couple of celebrities fell in love with it.
Simon Garfield: Queen Victoria wore it, but pretty much at the same time, maybe just before, uh, Empress Eugenie, who was the wife of Napoleon III, also found that this particular shade of mauve matched her eyes and wore it everywhere. And it was the Princess Diana effect or Jackie Kennedy effect. People saw it in the streets and word spread.
It became a mania.
Alexis Pedrick: Perkin’s mauve launched the hugely successful synthetic dye industry. Once you could do one color, you could pretty much do any color. Within 20 years, there were hundreds of new shades, all based on coal tar. They became known as aniline dyes. But even though chemists got more comfortable cozying up to industry, that didn’t mean they wholesale abandoned the idea of making something a tad more important.
Here’s Wallace Mendelson.
Wallace Mendelson: In any event, that was the beginning not only of discovery of one particular dye, it was really the beginning of what’s called synthetic organic chemistry.
Alexis Pedrick: So the failure to make a synthetic remedy for malaria launched a new field of chemistry. But we’re not at Thorazine yet.
We still need more people to fail, and coincidentally, they need to fail with another dye. And end up with another drug meant to treat, you guessed it, malaria.
Chapter Two. Methylene Blue.
By 1876, synthetic fabric dyes were fully in vogue. And color chemists were a fixture in the fabric industry. One of these was a chemist named Heinrich Caro.
Wallace Mendelson: He clearly viewed chemistry as being a very practical thing and was very interested in practical results of it.
Alexis Pedrick: Caro went to work as a chemist in a fabric factory that still used natural dyes and secret recipes, but he was young and excited about synthetic dyes. And so he pushed hard to make the switch.
In 1876, he synthesized a new bright blue fabric dye. Picture a quintessential blue blue. That’s Caro’s invention, methylene blue. It never achieved mauve level success, but eventually it did become a star when another chemist decided to dye something other than fabric with it.
Wallace Mendelson: Well, that story begins with Paul Ehrlich, who was born in 1854 in what is now Poland, was the son of an innkeeper and liquor distiller.
Alexis Pedrick: Paul Ehrlich had an older cousin who was a pathologist, and he’d been using aniline dyes to stain microscopic tissues. So, this was on his mind when he started his career.
And in 1886, he discovered that methylene blue stained the axons of neurons.
Wallace Mendelson: This was a very major step in making it possible to study the nervous system.
Alexis Pedrick: Nervous system tissue is transparent on a slide, but if you stain it blue, suddenly you can see it, you can study it. And this alone was hugely helpful, but something else happened when Ehrlich was looking at those slides.
He was using methylene blue to stain plasmodium parasites. These are the parasites that cause malaria.
Wallace Mendelson: By 1891, he and a colleague named Paul Guttmann found that methylene blue was actually toxic to plasmodium and they gave it to three patients in Berlin who improved and the plasmodium disappeared from their blood.
Alexis Pedrick: The story of synthetic dyes had come full circle. An attempt to make an antimalarial, that is, synthetic quinine, failed in the form of a beautiful purple fabric dye. 30 years later, a chemist discovers that a beautiful blue fabric dye is itself a useful antimalarial agent. We’re still not at Thorazine, but this itself was an important step.
Wallace Mendelson: So he began to think of dyes as, as therapeutic agents, which stained cell walls of bacteria and killed them or inhibited their ability to reproduce.
Alexis Pedrick: It wasn’t just that the dyes were the catalyst for the birth of the synthetic organic chemistry movement. The dyes themselves often had therapeutic properties.
Another dye, Prontosil Red, became a proto antibiotic. Because, remember, these synthetic dyes were made of chemical building blocks. Methylene Blue became the first synthetic drug, and it was used as an anti malarial all the way until World War II, when chloroquine emerged as a more effective treatment.
But Methylene Blue would find another life, again, because of some creative repurposing of another failure.
Chapter Three. Henri Laborit.
Laborit: Le premier est le comportement de consommation qui a soumis les besoins fondamentaux.
Alexis Pedrick: These are the words of Henri Laborit, a French surgeon, neurobiologist, writer, and philosopher.
Born in 1914, he defied typical labels and led a colorful life, doing things like interviewing Salvador Dali on television and making feature films about his philosophical ideas, like the one we just heard a clip of. Laborit was an army surgeon during World War II, and he was on a naval ship during the famous Dunkirk evacuation, when more than 300,000 Allied soldiers were rescued.
After World War II, he was stationed on a French naval base in Tunisia. And there, he returned to one of his interests, surgical shock. Now, surgical shock is a potentially fatal phenomenon, where patients blood pressure and circulation drop dramatically.
Wallace Mendelson: He viewed surgical shock, like many processes, probably was a basically healthy one, but when it got out of hand, it was too strong, then it become very harmful.
Alexis Pedrick: Laborit thought that the process of surgical shock was mediated by the release of the chemical histamine during surgery. So, he was interested in the new antihistamines that were being developed at the time.
Wallace Mendelson: Now, to get antihistamines, he approached a chemist named Paul Charpentier, who was busy developing antihistamines, most of which were derivatives of methylene blue.
Alexis Pedrick: Charpentier gave Laborit an antihistamine called promethazine. And when Laborit gave it to patients, it did two exciting things. First, it reduced the dose of anesthetics. And second, it made patients quiet. Laborit was thrilled by these results. But when he wrote to Charpentier for some more, Charpentier decided to send him something else.
Wallace Mendelson: Chlorpromazine, it had washed out as a malarial treatment, didn’t work, but it had very powerful anti histaminic chemical properties and it was known that it quieted animals.
Alexis Pedrick: He sent it to Laborit, who was now working at a hospital in Paris. And Laborit found that chlorpromazine worked as he had hoped.
It lowered patients body temperatures, something he called artificial hibernation, and calmed them down before surgery, decreasing the need for anesthetics. Now, if you’ve been following along, maybe you’re not surprised that a derivative of methylene blue ended up in Henri Laborit’s hands because of a failure.
Or, that Laborit turned this failure into not one, but two successes. Success number one, chlorpromazine solved the problem of surgical shock. But Laborit, ever thinking outside the box, wondered what else something like this could be used for.
We, the Mentally Ill: There are 118 patients in this one ward alone, a ward intended for only 60.
Some are more disturbed than others, and we’re all in each other’s ways. There are patients here that have been living in this ward for over 20 years. It’s crowded and smelly, but some don’t remember any other home.
Alexis Pedrick: In 1951, Laborit and his colleagues gave Chlorpromazine to a 24-year-old man diagnosed with mania. They found that in combination with barbiturates, the chlorpromazine calmed him down enough that he could leave the hospital after a few days. This could have been the moment that changed psychiatry forever.
Except for one small issue.
Wallace Mendelson: The problem was the psychiatric community wasn’t particularly interested. They had a number of treatments that they used, one of which was shock treatment. Others were packing patients in ice packs. And of course, psychotherapy was widely used. So his work didn’t get anywhere.
Alexis Pedrick: Psychiatry had never had any drugs before, so people were skeptical. But Laborit knew he was on to something.
Wallace Mendelson: And then one day, one of Laborit’s anesthesiologist colleagues said to him, you know, my brother in law is a famous psychiatrist at St. Anne’s and St. Anne’s was, was probably the most famous psychiatric hospital in France, if not in, in Europe in those years.
And why don’t we give some of this to my brother in law?
Alexis Pedrick: The brother in law convinced the hospital’s director to try it out. And the results stunned them.
Wallace Mendelson: The first thing they learned is you didn’t need to give barbiturates the way Laborit had. You could just give it by itself. And they quickly learned that the benefits of chlorpromazine didn’t seem to be related to lowering temperature. What they did discover was that it was very, very effective in not only in just quieting, but reducing the symptoms of psychosis, the disordered thinking, the hallucinations, and so on.
Alexis Pedrick: In 1952, chlorpromazine came out as an antipsychotic in France under the trade name Largactil. And in 1954, it came out in the United States as Thorazine.
Wallace Mendelson: This was a breakthrough. It made it possible for many patients who would have spent the rest of their lives in psychiatric care institutions to be able to be treated as outpatients.
Alexis Pedrick: And indeed, it was a derivative of methylene blue.
Chapter Four. Try again, fail again, fail better.
An anti malarial drug failed and became a dye. A dye failed and became an anti malarial drug. We tried to use the derivatives of that dye to make other kinds of anti malarials. And when that failed, we gave it to a guy who made deeply philosophical French films so that he could use it to treat surgical shock.
And then, even when we heard that derivative was good at calming psychiatric patients down, the psychiatry field responded with a collective, shrug emoji, only to change their minds because this French film guy, who also happened to be a neurobiologist, wouldn’t give up. And after all of that, I’m talking a hundred years worth of failures, the birth of a new field of chemistry, time and energy spent trying to solve a problem that wasn’t even anti psychotics.
And we finally got it. And you know what? It was amazing, but also not without complications. Remember Sally?
We, the Mentally Ill: I said goodbye to my doctor and I go to see my children again and my husband. I am very happy to go home.
Wallace Mendelson: Now there there’s of course a whole other story there, which is very often communities were not prepared to accept large numbers of previously hospitalized psychiatric patients, which presented its own set of problems.
Alexis Pedrick: After 1955, the number of patients institutionalized in asylums began to dwindle. Slowly at first, and then rapidly after 1965. Some patients, like Sally, went home. But for the rest, Thorazine was often used more as a control measure than as a therapeutic one.
Audio Archive: Stop forced drugging! Stop forced drugging!
Alexis Pedrick: This is Andrew Scull, the sociologist we heard from earlier in the episode.
Andrew Scull: Mental patients, because of their mental illness, were seen as people who couldn’t make rational choices about their treatment. They were locked away so they could be dealt with no matter what their protests were.
Giving people increasing doses of Thorazine just to see what would happen. Raising those doses to levels that we now know are very dangerous, that was all a feature early on.
Alexis Pedrick: We’d also later learn that Thorazine wasn’t exactly the miracle drug it was first touted to be.
Andrew Scull: The early studies on whether they were efficacious were completely uncontrolled, there were no, uh, comparison groups who weren’t getting the treatment, the person administering it was the one judging whether it worked.
There were all kinds of confounding things that help explain why in the early years drugs were seen as much more effective than they turn out to be.
Alexis Pedrick: You might be saying, was Thorazine even any better than what came before it? To which I will say, absolutely. Early treatments were brutal. Insulin induced comas, lobotomies, ice baths.
One renowned psychiatrist in New Jersey was even convinced that pulling teeth and removing organs was the key to solving psychosis. But a lot of things can be true all at once.
Andrew Scull: All of this history, in some sense, sort of hangs together, even though the drugs turn out to have some therapeutic value in certain patients, for some people.
Alexis Pedrick: Thorazine was revolutionary in 1954. There’d never been anything like it. And here’s the really disappointing part, there hasn’t really been anything revolutionary since. Antipsychotics haven’t progressed much since Thorazine. Schizophrenia drugs today are the descendants of Chlorpromazine, and they’re about as effective, though they do cause fewer harsh side effects.
Andrew Scull: But what they do create is a whole new set of side effects, particularly very pronounced weight gain, 30, 40, 50, 60 pounds in the space of a year or two. And then, as a consequence of that, or sometimes an unrelated set of issues, heart disease, diabetes, metabolic disorders, early death.
Alexis Pedrick: It’s estimated that two thirds of schizophrenia patients stop taking their medication.
The side effects are one reason, but another is that the current drugs only treat some schizophrenia symptoms. The ones that are known as the positive symptoms.
Andrew Scull: It’s odd language, right? So the positive symptoms are the very disturbing things, like the hallucinations and the delusions that characterize what we call schizophrenia.
And when these drugs work, they damp that down. They may not make them entirely disappear, but they become less overwhelming. And that’s the good thing that they do.
Alexis Pedrick: But schizophrenia also has what are called negative symptoms.
Andrew Scull: Loss of affect, loss of social contact, apathy, withdrawal, intellectual and emotional deterioration on a massive scale.
And the drugs don’t really do much for those things, which are among the most debilitating and life destroying aspects of that disorder.
Alexis Pedrick: So we’ve been at a decades long standstill. And it might be because, for the past 70 years, we’ve been going after the wrong drug target. Thorazine, and all its copycat and descendant drugs, work by affecting levels of a neurotransmitter called dopamine.
Andrew Miller: The field is almost taught as like, we don’t really know what the basis of schizophrenia is, but we have this dopamine hypothesis which fits with how current treatments work. And so you go out to talk to people and you’re like, well, if it’s not dopamine, it’s not going to work.
Alexis Pedrick: This is Andrew Miller, the inventor of a new schizophrenia drug. Instead of targeting dopamine receptors, it targets something called muscarinic receptors.
Andrew Miller: And that wasn’t in itself a new idea.
Alexis Pedrick: Andrew Miller didn’t start from scratch. He looked around for work that other scientists had already done, for something he could build off of, and he found it in a study that experimented with a molecule called Xanomeline for Alzheimer’s.
Andrew Miller: But what was most surprising about that original study was they discovered this very robust antipsychotic benefit in the subset of patients in that Alzheimer’s study who were experiencing hallucinations, delusions, and other symptoms of psychosis. And so that original sort of completely accidental discovery is what kind of started the whole field of muscarinic agonist based treatments for serious mental illness.
Alexis Pedrick: It was promising, but Xanomeline had too many intense GI side effects to be a successful drug. So, at the risk of making a major oversimplification, Andrew and his company, Karuna Therapeutics, combined Xanomeline with a generic drug used for bladder control, and voila! We have what might be the first successful novel schizophrenia drug in decades.
It’s called KarXT, and it’s shown a lot of promise in clinical trials. It works on both positive and negative symptoms, and it has minimal side effects.
Andrew Miller: I think with KarXT, there’s really the opportunity to introduce, for the first time in a really long time, a truly unique class of medicine for treating schizophrenia that’s not based on direct activity at, at dopamine or serotonin receptors, but interestingly enough, goes back to the same type of serendipitous human finding that has been, frankly, a really big source of historical innovation in psychiatry.
Alexis Pedrick: It’s kind of like Henri Laborit calling up Paul Charpentier and asking for the latest antihistamine or passing chlorpromazine on to his colleagues in the psychiatric department. If these stories are any indication, scientific success relies on collaboration.
And seeing promise in mistakes and failures. So, is KarXT finally something new? Has someone come along and turned sludge into something beautiful? Only time will tell. But if it fails, maybe they can take Samuel Beckett’s advice, and try again. Fail again. Fail better.
Distillations is produced by the Science History Institute. Our executive producer is Mariel Carr. Our producer is Rigoberto Hernandez. And our associate producer is Sarah Kaplan. This episode was reported by Mariel Carr and mixed by Jonathan Pfeffer, who also composed the theme music. This episode was inspired by our museum exhibit, Bold: Color from Test Tube to Textile.
You can learn more at sciencehistory.org/bold. You can find all our podcasts as well as videos and articles at sciencehistory.org/stories. And you can follow the science history Institute on Facebook, Twitter, and Instagram for news about our podcast and everything else going on in our free museum and library.
For Distillations, I’m Alexis Pedrick. Thanks for listening.