Frederick Banting, Charles Best, James Collip, and John Macleod
These four Toronto researchers discovered and purified insulin, creating a new and effective treatment for diabetes.
In the early 1920s Frederick Banting and Charles Best discovered insulin under the directorship of John Macleod at the University of Toronto. With the help of James Collip, insulin was purified, making it available for the successful treatment of diabetes. Banting and Macleod earned a Nobel Prize for their work in 1923.
At the turn of the 20th century, a strict low-calorie, no-carbohydrate diet was the only effective treatment for diabetes. But this method, with food intake sometimes as low as 500 calories per day, had its consequences, as slow starvation, like diabetes, drained patients of their strength and energy, leaving them semi-invalids. The diet treatment also required an inordinate amount of willpower on the part of the patient, very few of whom were able to maintain low-calorie diets over the long term.
In 1921 researchers at the University of Toronto began a series of experiments that would ultimately lead to the isolation and commercial production of insulin—a pancreatic hormone essential for metabolizing carbohydrates—and the successful treatment of diabetes.
Setting the Stage for the Discovery of Insulin
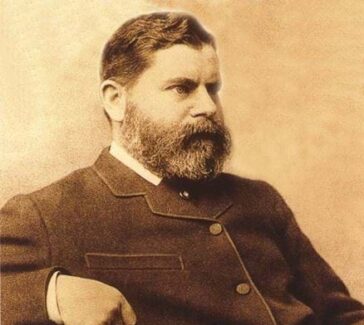
The connection between pancreatic secretions and diabetes was first shown in 1889 by two German physiologists at the University of Strasbourg, Oskar Minkowski and Joseph von Mering. While investigating the effect of pancreatic secretions on the metabolism of fat, they performed a complete pancreatectomy on a laboratory dog, only to discover that the animal developed a disease indistinguishable from diabetes.
Twenty years earlier a German medical student, Paul Langerhans, had discovered two systems of cells in the pancreas: the acini, which he knew produced the pancreatic digestive secretions, and another system whose function was unknown to him. These cells looked to Langerhans like tiny clusters of cells, or islands, floating among the acini.
In 1901 Eugene Opie, an American pathologist at Johns Hopkins University, made the association between the degeneration of these cells, which had been named the “islets of Langerhans,” and the onset of diabetes. Through the experimental efforts of these and many other researchers, the stage was set for the discovery of insulin—the hormonal antidiabetic secretion of the islets of Langerhans—in the first decades of the 20th century.
Frederick Banting
In 1920 Frederick Grant Banting (1891–1941) was a surgeon in a floundering practice in London, Ontario, Canada. The youngest son of Methodist farmers from Alliston, Ontario, Banting almost entered the Methodist ministry but decided at the last moment that his calling lay in medicine. World War I shortened his five-year medical course at the University of Toronto: his class did its entire fifth year during the summer of 1916 and, upon receiving their hasty degrees, went off to war.
Banting served as a battalion medical officer in the Canadian Army Medical Corps; he returned to Toronto in 1919 after having been wounded in the arm by shrapnel. He trained as a surgeon at the Hospital of Sick Children in Toronto, then decided to open a small practice as a surgeon in London, Ontario. Unfortunately, his earnings from his practice were meager, forcing him to take a position as a demonstrator in the local medical school. It was in this capacity that Banting was preparing a lecture about the function of the pancreas on October 30, 1920. He stopped at the medical school library, where he picked up the latest issue of Surgery, Gynecology and Obstetrics, and read an article titled “The Relation of the Islets of Langerhans to Diabetes, with Special Reference to Cases of Pancreatic Lithiasis.”
Banting Approaches John Macleod
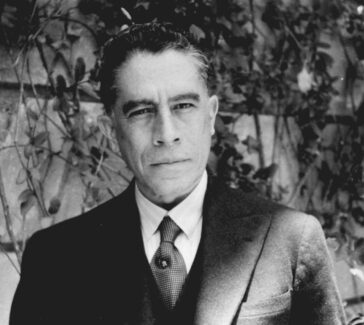
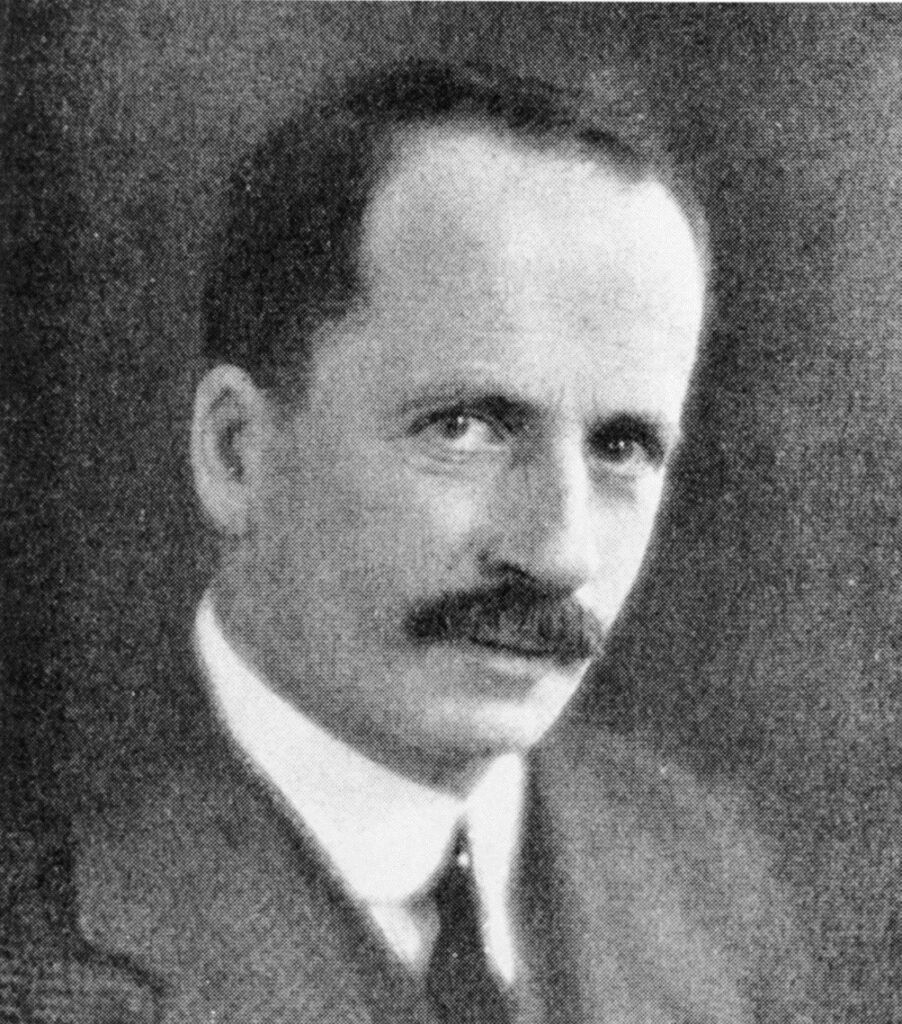
While thinking about pancreatic secretions after reading the article, Banting jotted down an idea for a preliminary experiment to further investigate the relationship between pancreatic secretions and diabetes. On November 7, following the advice of a colleague, Banting brought his idea to the attention of John James Rickard Macleod (1876–1935), a Scottish physiologist and expert in carbohydrate metabolism at his alma mater, the University of Toronto.
Macleod, the son of a minister, received his medical training at the University of Aberdeen and his biochemical training at the University of Leipzig. In 1903 Macleod emigrated to the United States to take a position as professor of physiology at Western Reserve University (now Case Western Reserve University) in Cleveland, Ohio. After 15 years at Western, Macleod accepted a professorship at the University of Toronto, where he conducted research on respiration.
Earlier in his career Macleod had published a series of papers on glycosuria, or the presence of sugar in the urine (a common indication of diabetes). As a scientist familiar with the literature on the subject, he was unimpressed with Banting’s range of knowledge about diabetes and the pancreas and skeptical about the soundness of Banting’s idea. However, Macleod decided to give him lab space, an assistant, and some laboratory dogs for two months at the end of the academic year.
Experiments Begin
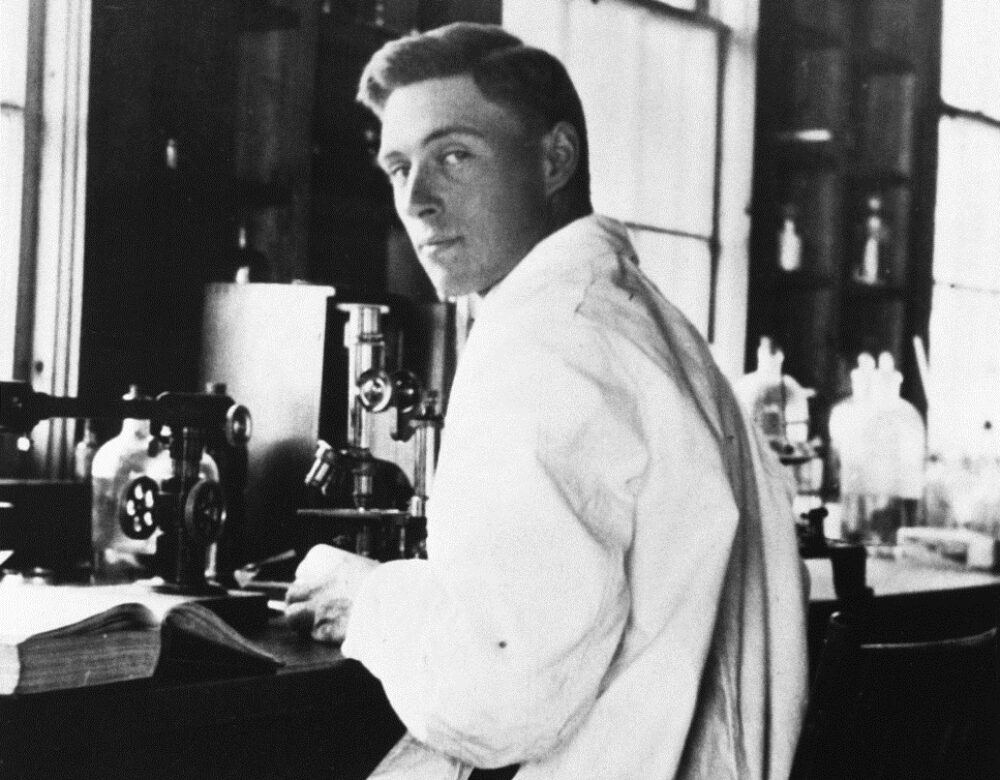
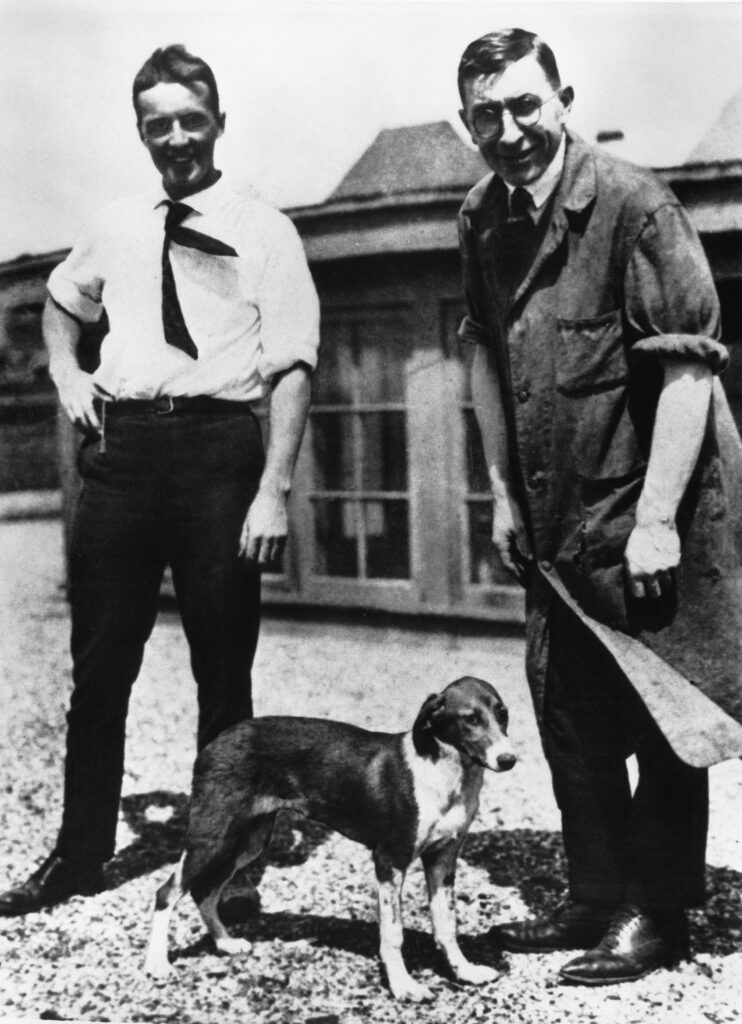
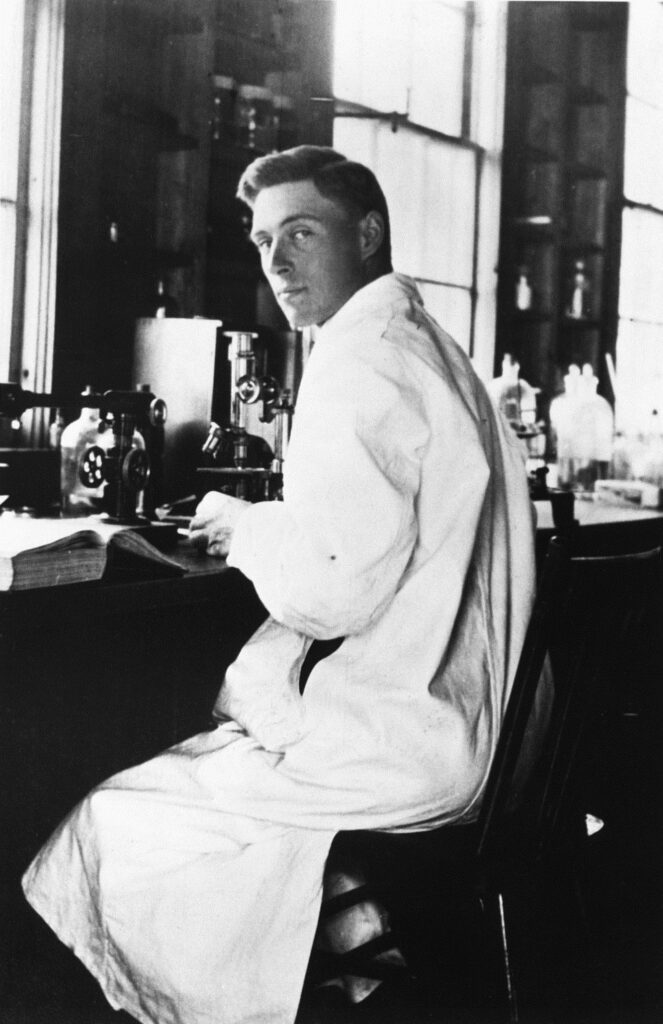
Banting and his assistant, Charles Herbert Best (1899–1978), began their experiments in May 1921. Best, the American son of Canadian parents, had just finished his bachelor’s degree in physiology and biochemistry at the University of Toronto and had been hired as a research assistant to Macleod, his former teacher. Macleod assigned him to Banting, and the 29-year-old surgeon and the 22-year-old assistant began their work together.
A combination of timing and good luck enabled the Toronto researchers to be the first to announce the discovery of insulin. Scientists in Germany and Hungary had come very close to finding pure insulin, but lack of funding and the devastation of World War I halted their progress. Following in the footsteps of earlier researchers, Banting and Best began to study diabetes through an experimental combination of duct ligation, which involved tying off the pancreatic duct to the small intestine, and pancreatectomies, or the complete surgical removal of the pancreas.
Duct ligation served to atrophy the acini cells that produced the digestive secretions, leaving behind only the cells of the islets of Langerhans. Duct-ligated dogs, it was discovered, did not develop diabetes. Pancreatectomy was the method of inducing diabetes: when all pancreatic tissue was removed, the experimental dogs immediately showed signs of glycosuria.
Banting’s idea of October 30 involved ligation of the pancreatic ducts of a dog and the extraction and isolation of whatever secretions were produced after the atrophy of the acini cells. He and Best began this experiment, only to find that it was difficult to keep duct-ligated, depancreatized dogs alive long enough to carry out any tests.
After a summer of many setbacks and failures, however, the team reported in the fall that they were keeping a severely diabetic dog alive with injections of an extract made from duct-ligated pancreas and prepared, following Macleod’s instructions, in saline. Amazingly, this extract dramatically lowered the blood sugar levels of diabetic experimental dogs.
Findings Are Presented and Tensions Begin
On December 30, 1921, Macleod, Banting, and Best presented their findings at the conference of the American Physiological Society, at Yale University. Banting, out of nervousness and inexperience, did a poor job delivering the paper, and the audience was highly critical of the findings presented. Macleod, as the chair of the session, joined the discussion in an attempt to rescue Banting from the scathing commentary. After this fiasco Banting became convinced that Macleod had stepped in to steal the credit from him and Best, and relations between the two began to deteriorate.
Purifying Insulin and the First Human Tests
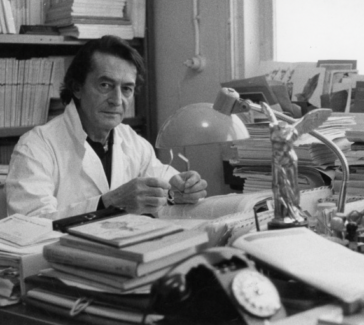
At the end of 1921 Macleod invited James Bertram Collip (1892–1965), a biochemist in the department of physiology at the University of Toronto, to help Banting and Best with purifying their extract. Collip, another University of Toronto graduate, was on sabbatical from the University of Alberta and, supported by a fellowship, had returned to his alma mater. As the experimental pace quickened, Banting and Best needed large amounts of their extract, and Collip set to work purifying the extract for clinical testing in humans.
The first clinical tests on a human patient were conducted on a severely diabetic 14-year-old boy. Although the injections of the extract failed to have resoundingly beneficial effects, the Toronto team continued to experiment. A short while later Collip made a breakthrough in purifying the extract, using alcohol in slightly over 90 percent concentration to precipitate out the active ingredient (insulin).
At the same time, though, personal tension was mounting among the four scientists, as Banting became increasingly bitter toward Macleod and pitted himself and Best against Collip in the race to purify the extract. At the end of January, Collip came to Banting and Best’s lab and informed the two that although he had discovered a method to produce pure extract, he would share it only with Macleod. It was only Best’s quick restraint that stopped Banting from attacking Collip.
Fortunately for the future of insulin an uneasy agreement made a few days later allowed them to continue to work together. On May 3, 1922, Macleod, representing the group, announced to the international medical community at a meeting of the Association of American Physicians that they had discovered “insulin”—the antidiabetic agent.
Nobel Prize
Banting and Macleod received the 1923 Nobel Prize in Physiology or Medicine for the discovery of insulin. That the Nobel committee chose only Banting and Macleod for the award caused more animosity. Banting, outraged that Macleod was chosen to share the prize with him, immediately announced that he would split his winnings with Best. Macleod, perhaps in reaction to Banting’s gesture, announced that he, too, would be splitting his award, with Collip.
By the end of 1923 insulin had been in commercial production for a year at the Eli Lilly and Company laboratories in Indianapolis. Diabetic patients who received insulin shots recovered from comas, resumed eating carbohydrates (in moderation), and realized they had been given a new lease on life.